Clinical Focus ›› 2025, Vol. 40 ›› Issue (7): 624-633.doi: 10.3969/j.issn.1004-583X.2025.07.007
Previous Articles Next Articles
Predictive value of platelet and white blood cell parameters for bronchopulmonary dysplasia in premature infants
Wang Xiaofang1,2, Cui Qingyang1( ), Liu Xinyu3
), Liu Xinyu3
- 1. Department of Pediatrics, the First Affiliated Hospital of Xinxiang Medical University, Weihui 453100, China
2. Department of Neonatology, Jincheng People's Hospital, Jincheng 048000, China
3. Family Planning Service Center of Shaodong Maternal and Child Health Hospital, Shaoyang 422000, China
-
Received:2025-03-07Online:2025-07-20Published:2025-07-17 -
Contact:Cui Qingyang E-mail:1282592772@qq.com
CLC Number:
Cite this article
Wang Xiaofang, Cui Qingyang, Liu Xinyu. Predictive value of platelet and white blood cell parameters for bronchopulmonary dysplasia in premature infants[J]. Clinical Focus, 2025, 40(7): 624-633.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: http://www.lchc.cn/EN/10.3969/j.issn.1004-583X.2025.07.007
| 组别 | 例数 | 性别[例(%)] | 住院时间 (d) | 胎龄 (d) | 出生体重 (g) | 母孕期合并疾病[例(%)] | 母绒毛膜羊膜炎[例(%)] | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | 是 | 否 | 是 | 否 | ||||||||||||||||||||||||||||
| BPD组 | 93 | 61(65.6) | 32(34.4) | 54.91±16.19 | 204.11±12.59 | 1179.46±256.23 | 70(75.3) | 23(24.7) | 1(1.1) | 92(98.9) | |||||||||||||||||||||||
| 非BPD组 | 165 | 84(50.9) | 81(49.1) | 42.82±11.98 | 210.67±8.78 | 1312.79±226.62 | 120(72.7) | 45(27.3) | 1(0.6) | 164(99.4) | |||||||||||||||||||||||
| χ2/t/Z值 | 5.209 | -6.371 | -4.445 | -4.326 | 0.198 | - | |||||||||||||||||||||||||||
| P值 | 0.022 | 0.000 | 0.000 | 0.000 | 0.656 | 1.000 | |||||||||||||||||||||||||||
| 组别 | 胎膜早破[例(%)] | 产前激素[例(%)] | 羊水情况[例(%)] | 胎盘[例(%)] | 脐带[例(%)] | ||||||||||||||||||||||||||||
| 是 | 否 | 是 | 否 | 正常 | 异常 | 正常 | 异常 | 正常 | 异常 | ||||||||||||||||||||||||
| BPD组 | 19(20.4) | 74(79.6) | 82(88.2) | 11(11.8) | 67(72.0) | 26(28.0) | 78(83.9) | 15(16.1) | 81(87.1) | 12(12.9) | |||||||||||||||||||||||
| 非BPD组 | 47(28.5) | 118(71.5) | 150(90.9) | 15(9.1) | 124(75.2) | 41(24.8) | 152(92.1) | 13(7.9) | 150(90.9) | 15(9.1) | |||||||||||||||||||||||
| χ2/t/Z值 | 2.027 | 0.492 | 0.299 | 4.184 | 0.923 | ||||||||||||||||||||||||||||
| P值 | 0.155 | 0.483 | 0.585 | 0.041 | 0.337 | ||||||||||||||||||||||||||||
| 组别 | Apgar评分(分) | 呼吸机(d) | PS使用情况[例(%)] | 合并疾病(PDA、PPHN、 ROP等)[例(%)] | |||||||||||||||||||||||||||||
| 1分钟 | 5分钟 | 10分钟 | 有创 | 无创 | 是 | 否 | 是 | 否 | |||||||||||||||||||||||||
| BPD组 | 6.68±2.38 | 8.19±1.87 | 9.74±0.74 | 9.37±12.78 | 20.40±15.69 | 81(87.1) | 12(12.9) | 41(44.1) | 52(55.9) | ||||||||||||||||||||||||
| 非BPD组 | 7.62±2.34 | 8.67±1.93 | 9.47±1.36 | 1.24±2.13 | 11.34±11.10 | 104(63.0) | 61(37.0) | 35(21.2) | 130(78.8) | ||||||||||||||||||||||||
| χ2/t/Z值 | -3.569 | -2.743 | -1.726 | -7.500 | -5.893 | 16.979 | 14.976 | ||||||||||||||||||||||||||
| P值 | 0.000 | 0.006 | 0.084 | 0.000 | 0.000 | 0.000 | 0.000 | ||||||||||||||||||||||||||
Tab.1 General information between groups
| 组别 | 例数 | 性别[例(%)] | 住院时间 (d) | 胎龄 (d) | 出生体重 (g) | 母孕期合并疾病[例(%)] | 母绒毛膜羊膜炎[例(%)] | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | 是 | 否 | 是 | 否 | ||||||||||||||||||||||||||||
| BPD组 | 93 | 61(65.6) | 32(34.4) | 54.91±16.19 | 204.11±12.59 | 1179.46±256.23 | 70(75.3) | 23(24.7) | 1(1.1) | 92(98.9) | |||||||||||||||||||||||
| 非BPD组 | 165 | 84(50.9) | 81(49.1) | 42.82±11.98 | 210.67±8.78 | 1312.79±226.62 | 120(72.7) | 45(27.3) | 1(0.6) | 164(99.4) | |||||||||||||||||||||||
| χ2/t/Z值 | 5.209 | -6.371 | -4.445 | -4.326 | 0.198 | - | |||||||||||||||||||||||||||
| P值 | 0.022 | 0.000 | 0.000 | 0.000 | 0.656 | 1.000 | |||||||||||||||||||||||||||
| 组别 | 胎膜早破[例(%)] | 产前激素[例(%)] | 羊水情况[例(%)] | 胎盘[例(%)] | 脐带[例(%)] | ||||||||||||||||||||||||||||
| 是 | 否 | 是 | 否 | 正常 | 异常 | 正常 | 异常 | 正常 | 异常 | ||||||||||||||||||||||||
| BPD组 | 19(20.4) | 74(79.6) | 82(88.2) | 11(11.8) | 67(72.0) | 26(28.0) | 78(83.9) | 15(16.1) | 81(87.1) | 12(12.9) | |||||||||||||||||||||||
| 非BPD组 | 47(28.5) | 118(71.5) | 150(90.9) | 15(9.1) | 124(75.2) | 41(24.8) | 152(92.1) | 13(7.9) | 150(90.9) | 15(9.1) | |||||||||||||||||||||||
| χ2/t/Z值 | 2.027 | 0.492 | 0.299 | 4.184 | 0.923 | ||||||||||||||||||||||||||||
| P值 | 0.155 | 0.483 | 0.585 | 0.041 | 0.337 | ||||||||||||||||||||||||||||
| 组别 | Apgar评分(分) | 呼吸机(d) | PS使用情况[例(%)] | 合并疾病(PDA、PPHN、 ROP等)[例(%)] | |||||||||||||||||||||||||||||
| 1分钟 | 5分钟 | 10分钟 | 有创 | 无创 | 是 | 否 | 是 | 否 | |||||||||||||||||||||||||
| BPD组 | 6.68±2.38 | 8.19±1.87 | 9.74±0.74 | 9.37±12.78 | 20.40±15.69 | 81(87.1) | 12(12.9) | 41(44.1) | 52(55.9) | ||||||||||||||||||||||||
| 非BPD组 | 7.62±2.34 | 8.67±1.93 | 9.47±1.36 | 1.24±2.13 | 11.34±11.10 | 104(63.0) | 61(37.0) | 35(21.2) | 130(78.8) | ||||||||||||||||||||||||
| χ2/t/Z值 | -3.569 | -2.743 | -1.726 | -7.500 | -5.893 | 16.979 | 14.976 | ||||||||||||||||||||||||||
| P值 | 0.000 | 0.006 | 0.084 | 0.000 | 0.000 | 0.000 | 0.000 | ||||||||||||||||||||||||||
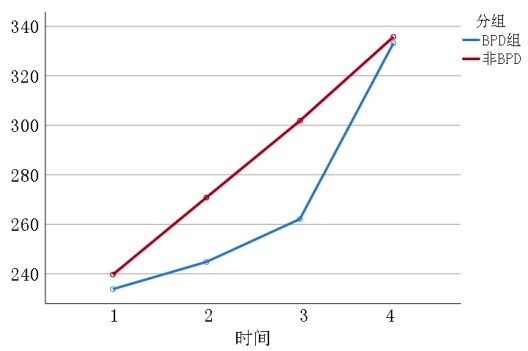
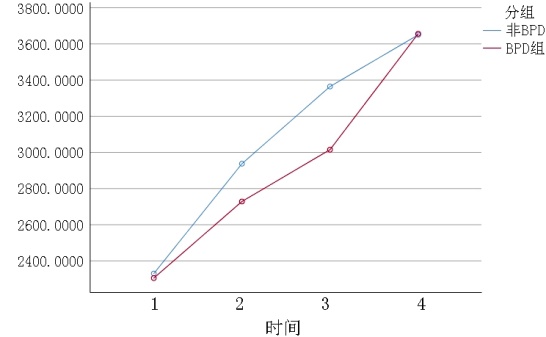
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 233.85±73.10 | 244.85±125.17 | 262.16±124.16*# | 333.19±126.46* |
| 非BPD组 | 165 | 239.73±66.82 | 270.87±113.68* | 301.85±133.02* | 335.74±123.32* |
| 组间 | F=2.990 P=0.096 | ||||
| 时点间 | F=57.391 P=0.000 | ||||
| 组间·时点间 | F=2.485 P=0.064 | ||||
Tab.2 PLT between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 233.85±73.10 | 244.85±125.17 | 262.16±124.16*# | 333.19±126.46* |
| 非BPD组 | 165 | 239.73±66.82 | 270.87±113.68* | 301.85±133.02* | 335.74±123.32* |
| 组间 | F=2.990 P=0.096 | ||||
| 时点间 | F=57.391 P=0.000 | ||||
| 组间·时点间 | F=2.485 P=0.064 | ||||
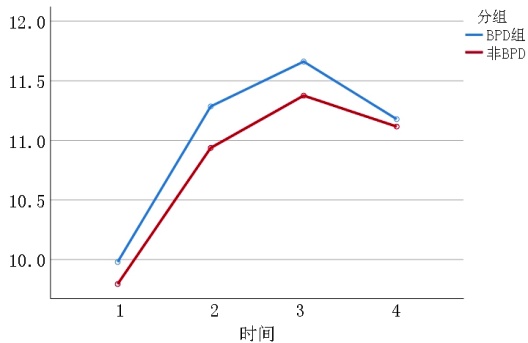
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 9.98±0.95 | 11.29±1.17*# | 11.66±1.11* | 11.18±1.01* |
| 非BPD组 | 165 | 9.80±1.77 | 10.94±1.35* | 11.38±1.31* | 11.12±1.26* |
| 组间 | F=3.039 P=0.082 | ||||
| 时点间 | F=115.192 P=0.000 | ||||
| 组间·时点间 | F=0.889 P=0.434 | ||||
Tab.3 MPV between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 9.98±0.95 | 11.29±1.17*# | 11.66±1.11* | 11.18±1.01* |
| 非BPD组 | 165 | 9.80±1.77 | 10.94±1.35* | 11.38±1.31* | 11.12±1.26* |
| 组间 | F=3.039 P=0.082 | ||||
| 时点间 | F=115.192 P=0.000 | ||||
| 组间·时点间 | F=0.889 P=0.434 | ||||
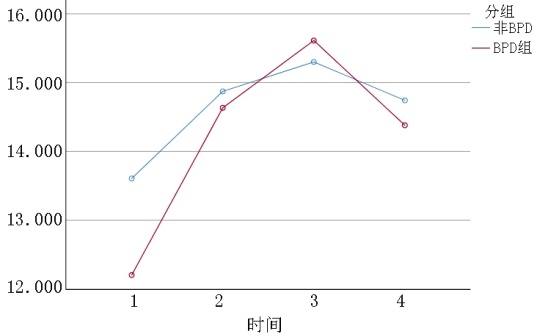
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 | |
|---|---|---|---|---|---|---|
| BPD组 | 93 | 12.20±2.88# | 14.63±3.33* | 15.61±2.78* | 14.38±2.80* | |
| 非BPD组 | 165 | 13.61±3.11 | 14.87±2.87* | 15.30±3.14* | 14.74±2.72* | |
| 组间 | F=1.956 P=0.163 | |||||
| 时点间 | F=62.641 P=0.000 | |||||
| 组间·时点间 | F=6.888 P=0.000 | |||||
Tab.4 PDW between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 | |
|---|---|---|---|---|---|---|
| BPD组 | 93 | 12.20±2.88# | 14.63±3.33* | 15.61±2.78* | 14.38±2.80* | |
| 非BPD组 | 165 | 13.61±3.11 | 14.87±2.87* | 15.30±3.14* | 14.74±2.72* | |
| 组间 | F=1.956 P=0.163 | |||||
| 时点间 | F=62.641 P=0.000 | |||||
| 组间·时点间 | F=6.888 P=0.000 | |||||
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 0.23±0.06 | 0.28±0.12* | 0.31±0.12* | 0.37±0.12* |
| 非BPD组 | 165 | 0.23±0.07 | 0.29±0.12* | 0.34±0.13* | 0.36±0.12* |
| 组间 | F=0.523 P=0.470 | ||||
| 时点间 | F=112.460 P=0.000 | ||||
| 组间·时点间 | F=2.423 P=0.068 | ||||
Tab.5 PCT between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 0.23±0.06 | 0.28±0.12* | 0.31±0.12* | 0.37±0.12* |
| 非BPD组 | 165 | 0.23±0.07 | 0.29±0.12* | 0.34±0.13* | 0.36±0.12* |
| 组间 | F=0.523 P=0.470 | ||||
| 时点间 | F=112.460 P=0.000 | ||||
| 组间·时点间 | F=2.423 P=0.068 | ||||
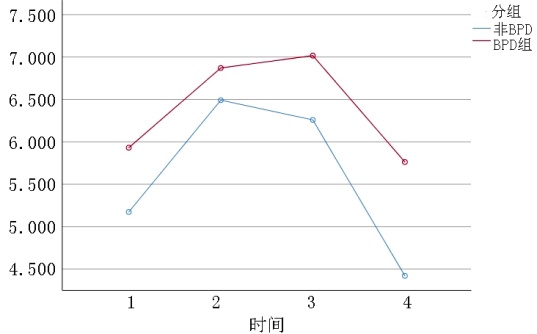
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 5.93±6.27 | 6.87±5.82 | 7.02±3.55 | 5.76±5.00# |
| 非BPD组 | 165 | 5.17±4.35 | 6.49±6.53* | 6.26±4.70* | 4.42±3.76 |
| 组间 | F=3.401 P=0.066 | ||||
| 时点间 | F=7.953 P=0.000 | ||||
| 组间·时点间 | F=0.496 P=0.671 | ||||
Tab.6 NEUC between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 5.93±6.27 | 6.87±5.82 | 7.02±3.55 | 5.76±5.00# |
| 非BPD组 | 165 | 5.17±4.35 | 6.49±6.53* | 6.26±4.70* | 4.42±3.76 |
| 组间 | F=3.401 P=0.066 | ||||
| 时点间 | F=7.953 P=0.000 | ||||
| 组间·时点间 | F=0.496 P=0.671 | ||||
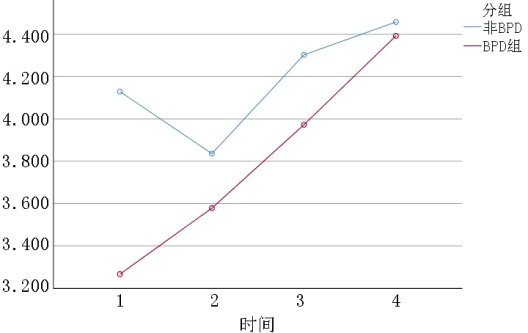
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 3.27±1.75# | 3.58±1.51 | 3.97±1.65* | 4.39±2.27* |
| 非BPD组 | 165 | 4.13±2.39 | 3.84±1.38 | 4.30±1.45 | 4.46±1.33 |
| 组间 | F=6.476 P=0.012 | ||||
| 时点间 | F=13.185 P=0.000 | ||||
| 组间·时点间 | F=3.059 P=0.039 | ||||
Tab.7 LYC between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 3.27±1.75# | 3.58±1.51 | 3.97±1.65* | 4.39±2.27* |
| 非BPD组 | 165 | 4.13±2.39 | 3.84±1.38 | 4.30±1.45 | 4.46±1.33 |
| 组间 | F=6.476 P=0.012 | ||||
| 时点间 | F=13.185 P=0.000 | ||||
| 组间·时点间 | F=3.059 P=0.039 | ||||
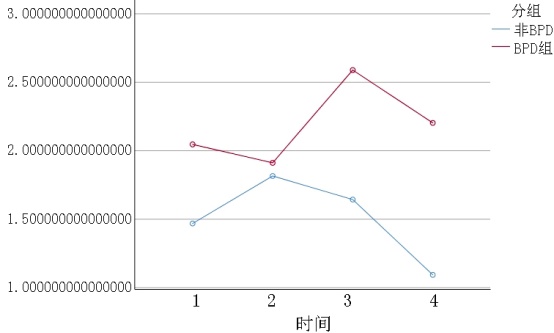
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 2.05±2.19# | 1.91±1.27 | 2.59±5.19# | 2.20±5.88# |
| 非BPD组 | 165 | 1.47±1.29 | 1.82±2.03 | 1.64±1.47 | 1.09±0.96 |
| 组间 | F=8.133 P=0.005 | ||||
| 时点间 | F=1.739 P=0.182 | ||||
| 组间·时点间 | F=2.193 P=0.121 | ||||
Tab.8 NLR between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 2.05±2.19# | 1.91±1.27 | 2.59±5.19# | 2.20±5.88# |
| 非BPD组 | 165 | 1.47±1.29 | 1.82±2.03 | 1.64±1.47 | 1.09±0.96 |
| 组间 | F=8.133 P=0.005 | ||||
| 时点间 | F=1.739 P=0.182 | ||||
| 组间·时点间 | F=2.193 P=0.121 | ||||
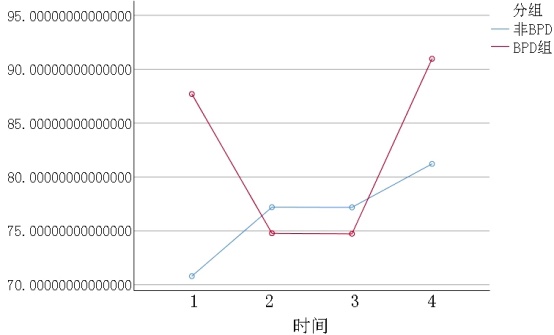
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 87.70±49.29# | 74.78±37.68* | 74.73±46.26* | 90.97±55.47 |
| 非BPD组 | 165 | 70.80±33.94 | 77.20±40.69 | 77.18±42.55 | 81.22±37.03* |
| 组间 | F=2.393 P=0.123 | ||||
| 时点间 | F=3.916 P=0.009 | ||||
| 组间·时点间 | F=3.929 P=0.009 | ||||
Tab.9 PLR between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 87.70±49.29# | 74.78±37.68* | 74.73±46.26* | 90.97±55.47 |
| 非BPD组 | 165 | 70.80±33.94 | 77.20±40.69 | 77.18±42.55 | 81.22±37.03* |
| 组间 | F=2.393 P=0.123 | ||||
| 时点间 | F=3.916 P=0.009 | ||||
| 组间·时点间 | F=3.929 P=0.009 | ||||
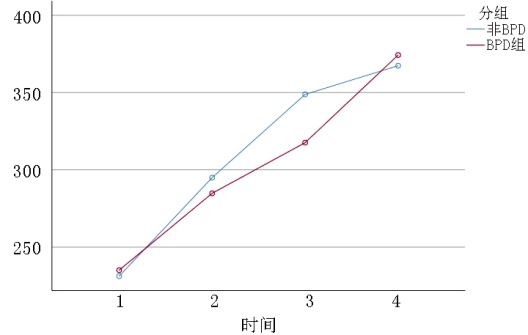
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 2304.85±676.98 | 2728.50±1305.44* | 3015.30±1367.43*# | 3656.52±1288.96* |
| 非BPD组 | 165 | 2330.02±714.99 | 2937.44±1227.73* | 3364.44±1336.12* | 3650.21±1182.26* |
| 组间 | F=1.790 P=0.182 | ||||
| 时点间 | F=87.097 P=0.000 | ||||
| 组间·时点间 | F=1.889 P=0.135 | ||||
Tab.10 PMI between groups
| 组别 | 例数 | 24 h | 1周 | 2周 | 4周 |
|---|---|---|---|---|---|
| BPD组 | 93 | 2304.85±676.98 | 2728.50±1305.44* | 3015.30±1367.43*# | 3656.52±1288.96* |
| 非BPD组 | 165 | 2330.02±714.99 | 2937.44±1227.73* | 3364.44±1336.12* | 3650.21±1182.26* |
| 组间 | F=1.790 P=0.182 | ||||
| 时点间 | F=87.097 P=0.000 | ||||
| 组间·时点间 | F=1.889 P=0.135 | ||||
| 影响因素 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 性别 | -0.846 | 0.330 | 6.590 | 0.010 | 0.429 | 0.225 | 0.819 |
| 胎龄(d) | -0.038 | 0.018 | 4.723 | 0.030 | 0.962 | 0.930 | 0.996 |
| 出生体重(g) | -0.002 | 0.001 | 5.007 | 0.025 | 0.998 | 0.997 | 1.000 |
| 胎盘 | 0.508 | 0.467 | 1.183 | 0.277 | 1.662 | 0.665 | 4.151 |
| Apgar评分1 min | -0.167 | 0.079 | 4.501 | 0.034 | 0.846 | 0.725 | 0.987 |
| Apgar评分10 min | 0.458 | 0.200 | 5.250 | 0.022 | 1.581 | 1.069 | 2.340 |
| PLT24 h内 | 0.026 | 0.019 | 1.808 | 0.179 | 1.026 | 0.988 | 1.066 |
| MPV24 h内 | 0.629 | 0.456 | 1.904 | 0.168 | 1.876 | 0.768 | 4.587 |
| PDW24 h内 | -0.096 | 0.058 | 2.758 | 0.097 | 0.908 | 0.811 | 1.017 |
| PCT24 h内 | 2.514 | 3.551 | 0.501 | 0.479 | 12.355 | 0.012 | 13026 |
| NEUC24 h内 | -0.012 | 0.070 | 0.029 | 0.865 | 0.988 | 0.862 | 1.133 |
| LYC24 h内 | -0.106 | 0.143 | 0.550 | 0.458 | 0.899 | 0.679 | 1.190 |
| NLR24 h内 | 0.047 | 0.216 | 0.048 | 0.826 | 1.049 | 0.687 | 1.600 |
| PLR24 h内 | 0.006 | 0.008 | 0.486 | 0.486 | 1.006 | 0.990 | 1.022 |
| PMI24 h内 | -0.003 | 0.002 | 2.083 | 0.149 | 0.997 | 0.993 | 1.001 |
| 常量 | 2.377 | 6.264 | 0.144 | 0.704 | 10.770 | - | - |
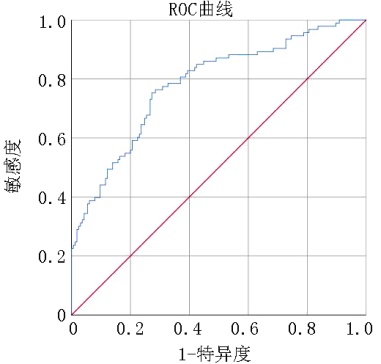
Tab.11 Logistic regression analysis of 24 hBPD
| 影响因素 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 性别 | -0.846 | 0.330 | 6.590 | 0.010 | 0.429 | 0.225 | 0.819 |
| 胎龄(d) | -0.038 | 0.018 | 4.723 | 0.030 | 0.962 | 0.930 | 0.996 |
| 出生体重(g) | -0.002 | 0.001 | 5.007 | 0.025 | 0.998 | 0.997 | 1.000 |
| 胎盘 | 0.508 | 0.467 | 1.183 | 0.277 | 1.662 | 0.665 | 4.151 |
| Apgar评分1 min | -0.167 | 0.079 | 4.501 | 0.034 | 0.846 | 0.725 | 0.987 |
| Apgar评分10 min | 0.458 | 0.200 | 5.250 | 0.022 | 1.581 | 1.069 | 2.340 |
| PLT24 h内 | 0.026 | 0.019 | 1.808 | 0.179 | 1.026 | 0.988 | 1.066 |
| MPV24 h内 | 0.629 | 0.456 | 1.904 | 0.168 | 1.876 | 0.768 | 4.587 |
| PDW24 h内 | -0.096 | 0.058 | 2.758 | 0.097 | 0.908 | 0.811 | 1.017 |
| PCT24 h内 | 2.514 | 3.551 | 0.501 | 0.479 | 12.355 | 0.012 | 13026 |
| NEUC24 h内 | -0.012 | 0.070 | 0.029 | 0.865 | 0.988 | 0.862 | 1.133 |
| LYC24 h内 | -0.106 | 0.143 | 0.550 | 0.458 | 0.899 | 0.679 | 1.190 |
| NLR24 h内 | 0.047 | 0.216 | 0.048 | 0.826 | 1.049 | 0.687 | 1.600 |
| PLR24 h内 | 0.006 | 0.008 | 0.486 | 0.486 | 1.006 | 0.990 | 1.022 |
| PMI24 h内 | -0.003 | 0.002 | 2.083 | 0.149 | 0.997 | 0.993 | 1.001 |
| 常量 | 2.377 | 6.264 | 0.144 | 0.704 | 10.770 | - | - |
| 影响因素 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 性别 | -0.604 | 0.325 | 3.451 | 0.063 | 0.547 | 0.289 | 1.034 |
| 胎龄(d) | -0.035 | 0.018 | 3.935 | 0.047 | 0.966 | 0.933 | 1.000 |
| 出生体重(g) | -0.002 | 0.001 | 3.622 | 0.057 | 0.998 | 0.997 | 1.000 |
| 胎盘 | 0.547 | 0.477 | 1.314 | 0.252 | 1.728 | 0.678 | 4.400 |
| Apgar评分1 min | -0.199 | 0.078 | 6.541 | 0.011 | 0.820 | 0.704 | 0.955 |
| Apgar评分10 min | 0.588 | 0.211 | 7.755 | 0.005 | 1.801 | 1.190 | 2.724 |
| PLT1周 | 0.021 | 0.014 | 2.440 | 0.118 | 1.022 | 0.995 | 1.049 |
| MPV1周 | 0.720 | 0.343 | 4.396 | 0.036 | 2.054 | 1.048 | 4.026 |
| PDW1周 | -0.069 | 0.063 | 1.199 | 0.273 | 0.933 | 0.824 | 1.056 |
| PCT1周 | 16.871 | 7.001 | 5.808 | 0.016 | 21232742 | 23.333 | 19321170966829 |
| NEUC1周 | 0.065 | 0.059 | 1.202 | 0.273 | 1.067 | 0.950 | 1.199 |
| LYC1周 | -0.161 | 0.235 | 0.468 | 0.494 | 0.851 | 0.537 | 1.350 |
| NLR1周 | -0.340 | 0.203 | 2.819 | 0.093 | 0.712 | 0.478 | 1.059 |
| PLR1周 | 0.003 | 0.008 | 0.120 | 0.730 | 1.003 | 0.987 | 1.019 |
| PMI1周 | -0.004 | 0.002 | 5.352 | 0.021 | 0.996 | 0.993 | 0.999 |
| 常量 | -1.424 | 5.391 | 0.070 | 0.792 | 0.241 | - | - |
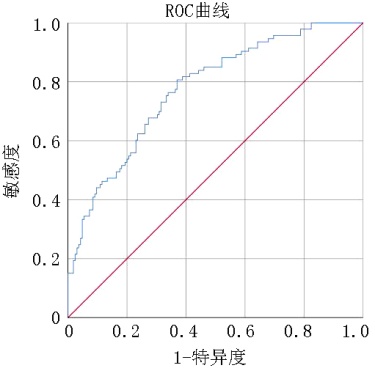
Tab.12 Logistic regression analysis of BPD at 1 week
| 影响因素 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 性别 | -0.604 | 0.325 | 3.451 | 0.063 | 0.547 | 0.289 | 1.034 |
| 胎龄(d) | -0.035 | 0.018 | 3.935 | 0.047 | 0.966 | 0.933 | 1.000 |
| 出生体重(g) | -0.002 | 0.001 | 3.622 | 0.057 | 0.998 | 0.997 | 1.000 |
| 胎盘 | 0.547 | 0.477 | 1.314 | 0.252 | 1.728 | 0.678 | 4.400 |
| Apgar评分1 min | -0.199 | 0.078 | 6.541 | 0.011 | 0.820 | 0.704 | 0.955 |
| Apgar评分10 min | 0.588 | 0.211 | 7.755 | 0.005 | 1.801 | 1.190 | 2.724 |
| PLT1周 | 0.021 | 0.014 | 2.440 | 0.118 | 1.022 | 0.995 | 1.049 |
| MPV1周 | 0.720 | 0.343 | 4.396 | 0.036 | 2.054 | 1.048 | 4.026 |
| PDW1周 | -0.069 | 0.063 | 1.199 | 0.273 | 0.933 | 0.824 | 1.056 |
| PCT1周 | 16.871 | 7.001 | 5.808 | 0.016 | 21232742 | 23.333 | 19321170966829 |
| NEUC1周 | 0.065 | 0.059 | 1.202 | 0.273 | 1.067 | 0.950 | 1.199 |
| LYC1周 | -0.161 | 0.235 | 0.468 | 0.494 | 0.851 | 0.537 | 1.350 |
| NLR1周 | -0.340 | 0.203 | 2.819 | 0.093 | 0.712 | 0.478 | 1.059 |
| PLR1周 | 0.003 | 0.008 | 0.120 | 0.730 | 1.003 | 0.987 | 1.019 |
| PMI1周 | -0.004 | 0.002 | 5.352 | 0.021 | 0.996 | 0.993 | 0.999 |
| 常量 | -1.424 | 5.391 | 0.070 | 0.792 | 0.241 | - | - |
| [1] |
|
| [2] |
doi: 10.1038/s41572-019-0127-7 pmid: 31727986 |
| [3] |
|
| [4] |
doi: 10.1186/s12890-022-01895-2 pmid: 35346143 |
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
张慧, 韩彤妍, 朴梅花, 等. 1 min低Apgar评分超早产儿/超低出生体重儿的远期结局[J]. 中华围产医学杂志, 2017, 20(5):366-370.
|
| [9] |
|
| [10] |
|
| [11] |
doi: 10.1007/s00431-025-06016-9 pmid: 40009187 |
| [12] |
doi: 10.1186/s12887-024-04868-y pmid: 38862972 |
| [13] |
|
| [14] |
|
| [15] |
doi: 10.1186/s12887-019-1515-6 pmid: 31039810 |
| [16] |
|
| [17] |
pmid: 10515876 |
| [18] |
doi: 10.3109/14767058.2015.1121475 pmid: 26697923 |
| [19] |
鲁炜慧, 徐莉敏, 吕勤, 等. 淋巴细胞亚群与早产儿支气管肺发育不良的关系[J]. 现代实用医学, 2019, 31(7):893-895.
|
| [20] |
杨智全, 王海青, 支更花, 等. TGF-β1水平和Treg数量对早产儿支气管肺发育不良的预测价值[J]. 临床和实验医学杂志, 2020, 19(1):85-88.
|
| [21] |
doi: 10.3389/fped.2019.00464 pmid: 31781524 |
| [22] |
|
| [23] |
doi: 10.1186/s40348-017-0076-8 pmid: 29116547 |
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
doi: 10.1182/blood-2017-12-823369 pmid: 29853539 |
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
doi: 10.17305/bb.2023.10135 pmid: 38236204 |
| [33] |
|
| [34] |
doi: 10.1038/nri.2017.105 pmid: 28990587 |
| [35] |
|
| [1] | Wei Jing, Cui Qingyang, Han Huizhen, Yan Huili, Liu Qingsheng. Serum level of IL-33 in premature infants with bronchopulmonary dysplasia complicated with pulmonary hypertension and its clinical significance [J]. Clinical Focus, 2025, 40(5): 445-449. |
| [2] | Zhao Yipin, Cui Qingyang. Analysis of risk factors for bronchopulmonary dysplasia in extremely premature/very low birth weight infants [J]. Clinical Focus, 2025, 40(1): 60-64. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||