Clinical Focus ›› 2025, Vol. 40 ›› Issue (5): 400-407.doi: 10.3969/j.issn.1004-583X.2025.05.003
Previous Articles Next Articles
Correlation of new inflammatory indicators in the complete blood count with major adverse cardiovascular events in patients with acute anterior wall ST-segment elevation myocardial infarction after percutaneous coronary intervention
Liu Ping1, Yu Meng1, Liu Mingxin1, Li Wenfeng2( )
)
- 1. Department of Cardiology, the First Affiliated Hospital of Jinzhou Medical University, Jinzhou 121000, China
2. Department of Cardiology, the First People's Hospital Jinzhou Dalian, Dalian 116100, China
-
Received:2024-12-16Online:2025-05-20Published:2025-05-23 -
Contact:Li Wenfeng E-mail:liwenfengqiuxue@163.com
CLC Number:
Cite this article
Liu Ping, Yu Meng, Liu Mingxin, Li Wenfeng. Correlation of new inflammatory indicators in the complete blood count with major adverse cardiovascular events in patients with acute anterior wall ST-segment elevation myocardial infarction after percutaneous coronary intervention[J]. Clinical Focus, 2025, 40(5): 400-407.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: http://www.lchc.cn/EN/10.3969/j.issn.1004-583X.2025.05.003
| 组别 | 例数 | 年龄(岁) | 性别[例(%)] | 既往史[例(%)] | 入院心率 (次/min) | 入院收缩压 (mmHg) | 入院舒张压 (mmHg) | BMI (kg/m2) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男性 | 女性 | 糖尿病 | 高血压 | 吸烟史 | ||||||||||||||||||||
| MACE组 | 95 | 62.43±13.52 | 67(70.5) | 28(29.5) | 21(22.0) | 45(47.0) | 55(58.0) | 78.57±12.26 | 122.51±25.75 | 75.03±19.22 | 24.70±3.13 | |||||||||||||
| 非MACE组 | 227 | 60.53±11.44 | 166(73.1) | 61(26.9) | 47(21.0) | 111(49.0) | 126(56.0) | 76.37±11.68 | 135.51±23.72 | 80.74±14.53 | 24.54±3.49 | |||||||||||||
| t/Z/χ2值 | -1.288 | 0.227 | 0.079 | 0.063 | 0.155 | -1.546 | 4.373 | 2.908 | -0.376 | |||||||||||||||
| P值 | 0.199 | 0.634 | 0.779 | 0.802 | 0.694 | 0.139 | <0.001 | 0.010 | 0.707 | |||||||||||||||
| 组别 | 左室射血分数 (%) | 左室每搏输出量 (ml) | 左房内径 (mm) | 左室收缩末期内径 (mm) | 左室舒张末期内径 (mm) | BNP (pg/ml) | 总胆固醇 (mmol/L) | |||||||||||||||||
| MACE组 | 49.00(43.00, 58.00) | 57.00(51.00, 67.00) | 36.00(34.00, 39.00) | 46.00(44.00, 48.00) | 31.00(30.00, 32.00) | 203.70(42.40, 527.40) | 4.56±0.91 | |||||||||||||||||
| 非MACE组 | 54.00(45.00, 58.00) | 59.00(53.00, 64.00) | 36.00(34.00, 38.00) | 46.00(43.00, 48.00) | 31.00(30.00, 32.00) | 74.60(23.40, 190.40) | 4.73±1.02 | |||||||||||||||||
| t/Z/χ2值 | -1.893 | -0.427 | -0.076 | -0.304 | -0.233 | -4.162 | 1.450 | |||||||||||||||||
| P值 | 0.058 | 0.669 | 0.939 | 0.761 | 0.816 | <0.001 | 0.148 | |||||||||||||||||
| 组别 | 甘油三酯 (mmol/L) | 低密度脂蛋白 胆固醇(mmol/L) | 高密度脂蛋白 胆固醇(mmol/L) | 血肌酐 (mmol/L) | 尿酸 (μmol/L) | 白细胞计数 (×109/L) | ||||||||||||||||||
| MACE组 | 1.15(0.69, 1.72) | 3.10(2.73, 3.67) | 1.08(0.90, 1.22) | 77.50(68.30, 96.40) | 331.90(269.30, 421.88) | 11.39(8.56, 16.79) | ||||||||||||||||||
| 非MACE组 | 1.41(0.92, 1.96) | 2.90(2.47, 3.47) | 1.04(0.91, 1.19) | 71.50(62.30, 81.00) | 319.00(248.30, 375.65) | 8.54(6.95, 10.11) | ||||||||||||||||||
| t/Z/χ2值 | -2.751 | -1.059 | -0.610 | -0.548 | -2.160 | -0.984 | ||||||||||||||||||
| P值 | 0.006 | 0.036 | 0.542 | 0.001 | 0.031 | <0.001 | ||||||||||||||||||
| 组别 | 中性粒细胞计数 (×109/L) | 单核粒细胞计数 (×109/L) | 淋巴细胞计数 (×109/L) | 血红蛋白 (g/L) | 血小板计数 (×109/L) | 丙氨酸氨基转移酶 (U/L) | ||||||||||||||||||
| MACE组 | 11.36(8.29, 15.95) | 0.85(0.67, 1.10) | 1.11(0.91, 1.80) | 139.00(126.00, 150.00) | 256.40(211.10, 313.60) | 13.00(16.00, 23.50) | ||||||||||||||||||
| 非MACE组 | 7.09(5.61, 8.64) | 0.71(0.59, 0.87) | 1.57(1.21, 2.06) | 138.00(122.00, 147.00) | 214.10(183.20, 256.30) | 13.00(16.00, 24.00) | ||||||||||||||||||
| t/Z/χ2值 | -9.047 | -4.548 | 4.168 | -0.662 | -5.431 | -3.388 | ||||||||||||||||||
| P值 | <0.001 | <0.001 | 0.001 | 0.507 | <0.001 | 0.509 | ||||||||||||||||||
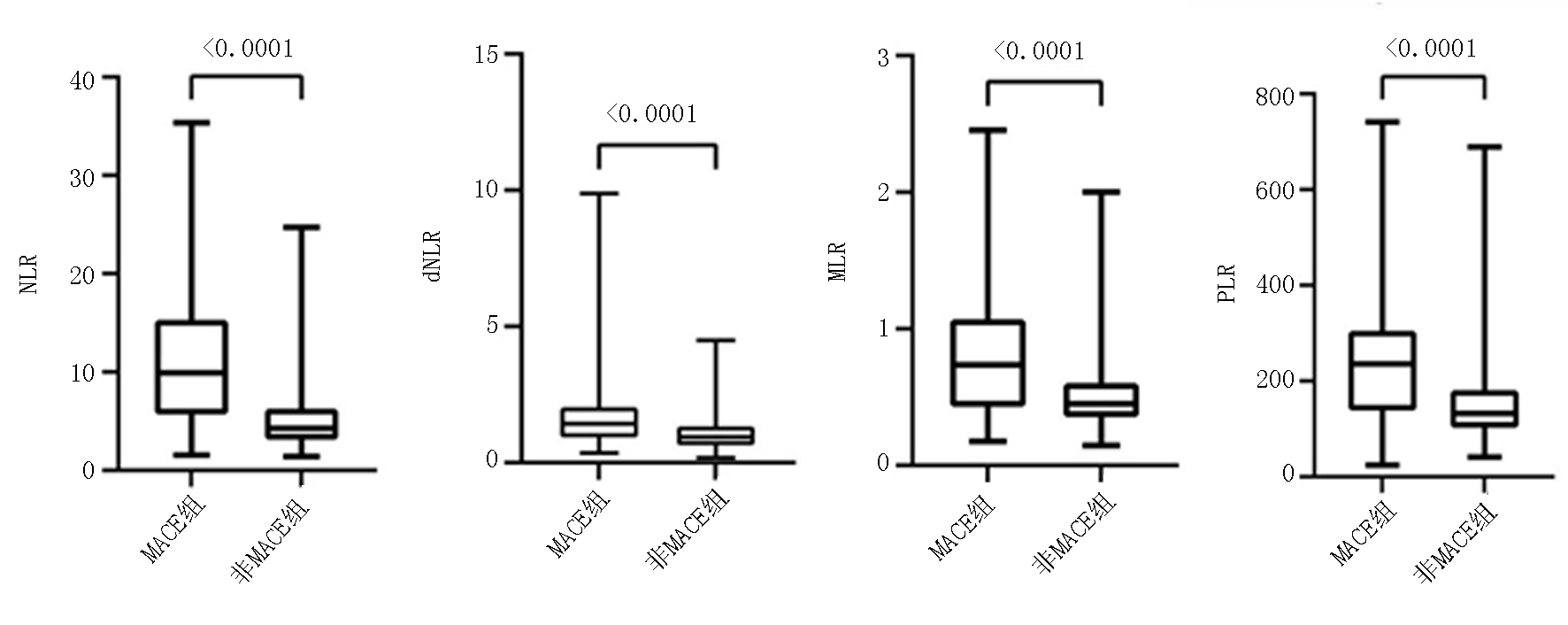
| 组别 | 天冬氨酸氨基转移酶 (U/L) | 白蛋白 (g/L) | NLR | dNLR | MLR | PLR | ||||||||||||||||||
| MACE组 | 18.00(15.00, 22.50) | 39.90(37.40, 41.70) | 11.51±7.43 | 1.83±1.50 | 0.86±0.54 | 237.50±133.34 | ||||||||||||||||||
| 非MACE组 | 18.00(14.50, 23.50) | 39.30(37.40, 41.00) | 5.32±3.52 | 1.08±0.62 | 0.50±0.23 | 154.31±88.50 | ||||||||||||||||||
| t/Z/χ2值 | -2.390 | -0.362 | -10.137 | -6.317 | -8.428 | -6.564 | ||||||||||||||||||
| P值 | 0.676 | 0.714 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||||||
Tab.1 Comparison of baseline clinical data between the MACE group and the non-MACE group
| 组别 | 例数 | 年龄(岁) | 性别[例(%)] | 既往史[例(%)] | 入院心率 (次/min) | 入院收缩压 (mmHg) | 入院舒张压 (mmHg) | BMI (kg/m2) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男性 | 女性 | 糖尿病 | 高血压 | 吸烟史 | ||||||||||||||||||||
| MACE组 | 95 | 62.43±13.52 | 67(70.5) | 28(29.5) | 21(22.0) | 45(47.0) | 55(58.0) | 78.57±12.26 | 122.51±25.75 | 75.03±19.22 | 24.70±3.13 | |||||||||||||
| 非MACE组 | 227 | 60.53±11.44 | 166(73.1) | 61(26.9) | 47(21.0) | 111(49.0) | 126(56.0) | 76.37±11.68 | 135.51±23.72 | 80.74±14.53 | 24.54±3.49 | |||||||||||||
| t/Z/χ2值 | -1.288 | 0.227 | 0.079 | 0.063 | 0.155 | -1.546 | 4.373 | 2.908 | -0.376 | |||||||||||||||
| P值 | 0.199 | 0.634 | 0.779 | 0.802 | 0.694 | 0.139 | <0.001 | 0.010 | 0.707 | |||||||||||||||
| 组别 | 左室射血分数 (%) | 左室每搏输出量 (ml) | 左房内径 (mm) | 左室收缩末期内径 (mm) | 左室舒张末期内径 (mm) | BNP (pg/ml) | 总胆固醇 (mmol/L) | |||||||||||||||||
| MACE组 | 49.00(43.00, 58.00) | 57.00(51.00, 67.00) | 36.00(34.00, 39.00) | 46.00(44.00, 48.00) | 31.00(30.00, 32.00) | 203.70(42.40, 527.40) | 4.56±0.91 | |||||||||||||||||
| 非MACE组 | 54.00(45.00, 58.00) | 59.00(53.00, 64.00) | 36.00(34.00, 38.00) | 46.00(43.00, 48.00) | 31.00(30.00, 32.00) | 74.60(23.40, 190.40) | 4.73±1.02 | |||||||||||||||||
| t/Z/χ2值 | -1.893 | -0.427 | -0.076 | -0.304 | -0.233 | -4.162 | 1.450 | |||||||||||||||||
| P值 | 0.058 | 0.669 | 0.939 | 0.761 | 0.816 | <0.001 | 0.148 | |||||||||||||||||
| 组别 | 甘油三酯 (mmol/L) | 低密度脂蛋白 胆固醇(mmol/L) | 高密度脂蛋白 胆固醇(mmol/L) | 血肌酐 (mmol/L) | 尿酸 (μmol/L) | 白细胞计数 (×109/L) | ||||||||||||||||||
| MACE组 | 1.15(0.69, 1.72) | 3.10(2.73, 3.67) | 1.08(0.90, 1.22) | 77.50(68.30, 96.40) | 331.90(269.30, 421.88) | 11.39(8.56, 16.79) | ||||||||||||||||||
| 非MACE组 | 1.41(0.92, 1.96) | 2.90(2.47, 3.47) | 1.04(0.91, 1.19) | 71.50(62.30, 81.00) | 319.00(248.30, 375.65) | 8.54(6.95, 10.11) | ||||||||||||||||||
| t/Z/χ2值 | -2.751 | -1.059 | -0.610 | -0.548 | -2.160 | -0.984 | ||||||||||||||||||
| P值 | 0.006 | 0.036 | 0.542 | 0.001 | 0.031 | <0.001 | ||||||||||||||||||
| 组别 | 中性粒细胞计数 (×109/L) | 单核粒细胞计数 (×109/L) | 淋巴细胞计数 (×109/L) | 血红蛋白 (g/L) | 血小板计数 (×109/L) | 丙氨酸氨基转移酶 (U/L) | ||||||||||||||||||
| MACE组 | 11.36(8.29, 15.95) | 0.85(0.67, 1.10) | 1.11(0.91, 1.80) | 139.00(126.00, 150.00) | 256.40(211.10, 313.60) | 13.00(16.00, 23.50) | ||||||||||||||||||
| 非MACE组 | 7.09(5.61, 8.64) | 0.71(0.59, 0.87) | 1.57(1.21, 2.06) | 138.00(122.00, 147.00) | 214.10(183.20, 256.30) | 13.00(16.00, 24.00) | ||||||||||||||||||
| t/Z/χ2值 | -9.047 | -4.548 | 4.168 | -0.662 | -5.431 | -3.388 | ||||||||||||||||||
| P值 | <0.001 | <0.001 | 0.001 | 0.507 | <0.001 | 0.509 | ||||||||||||||||||
| 组别 | 天冬氨酸氨基转移酶 (U/L) | 白蛋白 (g/L) | NLR | dNLR | MLR | PLR | ||||||||||||||||||
| MACE组 | 18.00(15.00, 22.50) | 39.90(37.40, 41.70) | 11.51±7.43 | 1.83±1.50 | 0.86±0.54 | 237.50±133.34 | ||||||||||||||||||
| 非MACE组 | 18.00(14.50, 23.50) | 39.30(37.40, 41.00) | 5.32±3.52 | 1.08±0.62 | 0.50±0.23 | 154.31±88.50 | ||||||||||||||||||
| t/Z/χ2值 | -2.390 | -0.362 | -10.137 | -6.317 | -8.428 | -6.564 | ||||||||||||||||||
| P值 | 0.676 | 0.714 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||||||
| 变量 | 单因素logistic回归分析 | 多因素logistic回归分析 | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | 95%CI | P值 | OR值 | 95%CI | P值 | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| NLR | 3.552 | 2.516 | 5.014 | <0.001 | 2.232 | 1.233 | 4.041 | 0.008 |
| dNLR | 2.462 | 1.732 | 3.398 | <0.001 | 2.128 | 1.398 | 3.237 | 0.015 |
| MLR | 2.840 | 2.038 | 3.956 | <0.001 | 1.764 | 1.118 | 2.785 | <0.001 |
| PLR | 2.179 | 1.644 | 2.889 | <0.001 | 0.970 | 0.599 | 1.572 | 0.903 |
Tab.2 Univariate and multivariate logistic regression analysis of four indicators in predicting MACEs
| 变量 | 单因素logistic回归分析 | 多因素logistic回归分析 | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | 95%CI | P值 | OR值 | 95%CI | P值 | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| NLR | 3.552 | 2.516 | 5.014 | <0.001 | 2.232 | 1.233 | 4.041 | 0.008 |
| dNLR | 2.462 | 1.732 | 3.398 | <0.001 | 2.128 | 1.398 | 3.237 | 0.015 |
| MLR | 2.840 | 2.038 | 3.956 | <0.001 | 1.764 | 1.118 | 2.785 | <0.001 |
| PLR | 2.179 | 1.644 | 2.889 | <0.001 | 0.970 | 0.599 | 1.572 | 0.903 |
| 变量 | 高血压组(n=156) | 非高血压组(n=166) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | 95%CI | P值 | OR值 | 95%CI | P值 | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| NLR | 2.957 | 1.135 | 7.704 | 0.027 | 1.623 | 0.728 | 3.617 | 0.236 |
| dNLR | 1.256 | 0.689 | 2.293 | 0.457 | 2.646 | 1.539 | 4.548 | <0.001 |
| MLR | 1.827 | 0.924 | 3.613 | 0.083 | 1.899 | 1.012 | 3.613 | 0.043 |
| PLR | 1.183 | 0.631 | 2.216 | 0.600 | 0.833 | 0.398 | 1.745 | 0.629 |
Tab.3 The correlation of four indicators with in-hospital MACEs after PCI in STEMI patients in the hypertension subgroup and non-hypertension subgroup
| 变量 | 高血压组(n=156) | 非高血压组(n=166) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | 95%CI | P值 | OR值 | 95%CI | P值 | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| NLR | 2.957 | 1.135 | 7.704 | 0.027 | 1.623 | 0.728 | 3.617 | 0.236 |
| dNLR | 1.256 | 0.689 | 2.293 | 0.457 | 2.646 | 1.539 | 4.548 | <0.001 |
| MLR | 1.827 | 0.924 | 3.613 | 0.083 | 1.899 | 1.012 | 3.613 | 0.043 |
| PLR | 1.183 | 0.631 | 2.216 | 0.600 | 0.833 | 0.398 | 1.745 | 0.629 |
| 变量 | 糖尿病组(n=68) | 非糖尿病组(n=254) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | 95%CI | P值 | OR值 | 95%CI | P值 | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| NLR | 3.970 | 0.525 | 9.971 | 0.182 | 2.288 | 1.146 | 4.570 | 0.019 |
| dNLR | 3.752 | 0.532 | 9.753 | 0.575 | 1.854 | 1.125 | 3.056 | 0.015 |
| MLR | 1.799 | 0.322 | 9.819 | 0.509 | 1.859 | 1.148 | 3.012 | 0.012 |
| PLR | 3.703 | 0.734 | 8.688 | 0.113 | 0.806 | 0.447 | 1.452 | 0.472 |
Tab.4 The correlation of four indicators and in-hospital MACEs after PCI in STEMI patients in the diabetes and non-diabetes subgroups
| 变量 | 糖尿病组(n=68) | 非糖尿病组(n=254) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | 95%CI | P值 | OR值 | 95%CI | P值 | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| NLR | 3.970 | 0.525 | 9.971 | 0.182 | 2.288 | 1.146 | 4.570 | 0.019 |
| dNLR | 3.752 | 0.532 | 9.753 | 0.575 | 1.854 | 1.125 | 3.056 | 0.015 |
| MLR | 1.799 | 0.322 | 9.819 | 0.509 | 1.859 | 1.148 | 3.012 | 0.012 |
| PLR | 3.703 | 0.734 | 8.688 | 0.113 | 0.806 | 0.447 | 1.452 | 0.472 |
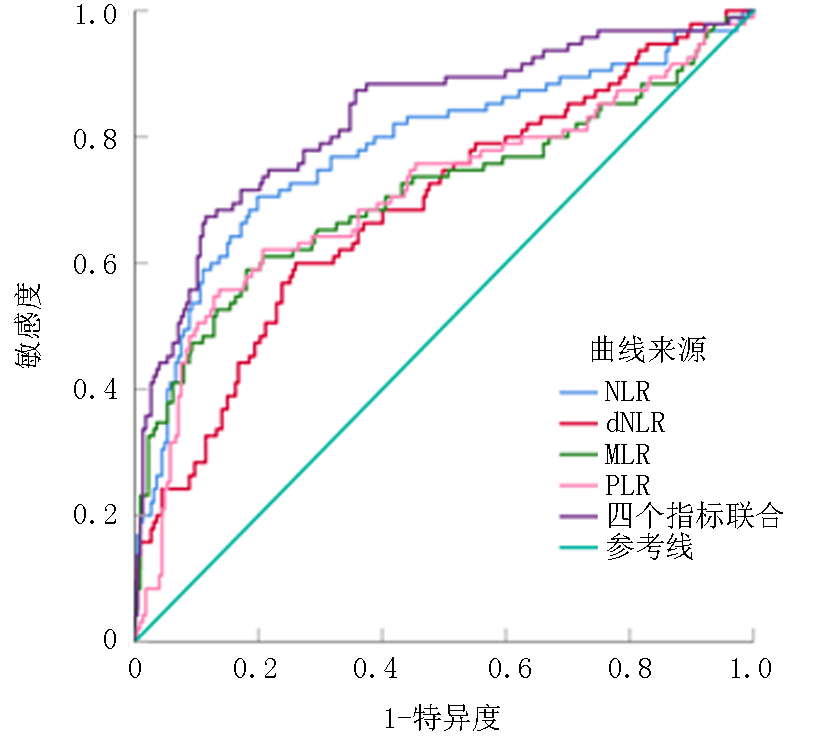
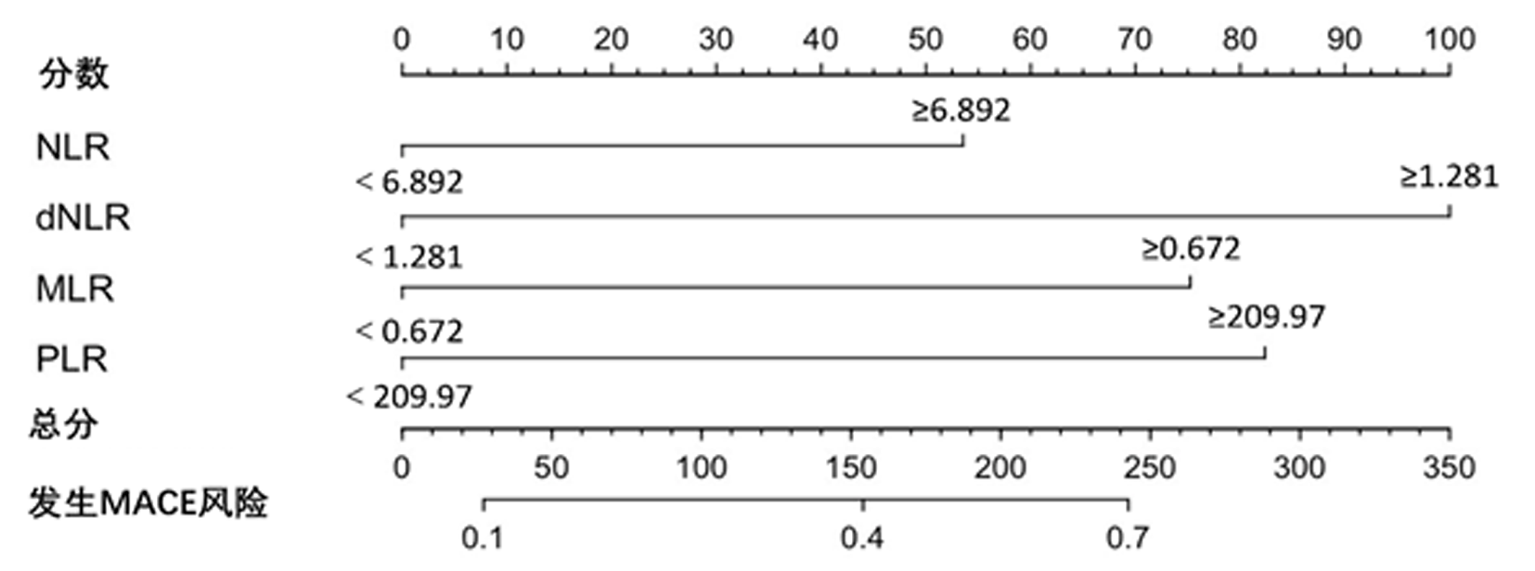
| 变量 | 界值 | AUC | P值 | 95%CI | 敏感度 (%) | 特异度 (%) | ROC曲线分析 | ||
|---|---|---|---|---|---|---|---|---|---|
| 下限 | 上限 | AUC差异 | P值 | ||||||
| NLR | 6.892 | 0.781 | <0.001 | 0.720 | 0.843 | 70.5 | 80.2 | 0.049 | 0.018 |
| dNLR | 1.281 | 0.687 | <0.001 | 0.622 | 0.753 | 60.0 | 74.0 | 0.144 | <0.001 |
| MLR | 0.672 | 0.711 | <0.001 | 0.641 | 0.781 | 58.9 | 81.9 | 0.120 | <0.001 |
| PLR | 209.970 | 0.708 | <0.001 | 0.639 | 0.777 | 55.8 | 86.3 | 0.123 | <0.001 |
| 四者联合 | - | 0.831 | <0.001 | 0.751 | 0.863 | 67.4 | 88.5 | 参考 | 参考 |
Tab.5 Predictive value of the combination of four inflammatory indicators in in-hospital MACEs in STEMI patients after PCI
| 变量 | 界值 | AUC | P值 | 95%CI | 敏感度 (%) | 特异度 (%) | ROC曲线分析 | ||
|---|---|---|---|---|---|---|---|---|---|
| 下限 | 上限 | AUC差异 | P值 | ||||||
| NLR | 6.892 | 0.781 | <0.001 | 0.720 | 0.843 | 70.5 | 80.2 | 0.049 | 0.018 |
| dNLR | 1.281 | 0.687 | <0.001 | 0.622 | 0.753 | 60.0 | 74.0 | 0.144 | <0.001 |
| MLR | 0.672 | 0.711 | <0.001 | 0.641 | 0.781 | 58.9 | 81.9 | 0.120 | <0.001 |
| PLR | 209.970 | 0.708 | <0.001 | 0.639 | 0.777 | 55.8 | 86.3 | 0.123 | <0.001 |
| 四者联合 | - | 0.831 | <0.001 | 0.751 | 0.863 | 67.4 | 88.5 | 参考 | 参考 |
| [1] |
Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC guidelines for the management of acute coronary syndromes[J]. Eur Heart J, 2023, 44(38):3720-3826.
doi: 10.1093/eurheartj/ehad191 pmid: 37622654 |
| [2] |
Bhatt DL, Lopes RD, Harrington RA. Diagnosis and treatment of acute coronary syndromes: A review[J]. JAMA, 2022, 327(7):662-675.
doi: 10.1001/jama.2022.0358 pmid: 35166796 |
| [3] | Martin SS, Aday AW, Almarzooq ZI, et al. 2024 heart disease and stroke statistics: A report of US and global data from the American Heart Association[J]. Circulation, 2024, 149(8):e347-e913. |
| [4] | 国家心血管病中心, 中国心血管健康与疾病报告编写组. 《中国心血管健康与疾病报告》2023(冠心病部分内容)[J]. 心肺血管病杂志, 2024, 43(10):1015-1024. |
| [5] |
Jia X, Buckley L, Sun C, et al. Association of interleukin-6 and interleukin-18 with cardiovascular disease in older adults: Atherosclerosis risk in communities study[J]. Eur J Prev Cardiol, 2023, 30(16):1731-1740.
doi: 10.1093/eurjpc/zwad197 pmid: 37306504 |
| [6] | Vinayak M, Cao D, Tanner R, et al. Impact of bleeding risk and inflammation on cardiovascular outcomes after percutaneous coronary intervention[J]. JACC Cardiovasc Interv, 2024, 17(3):345-355. |
| [7] | 陈建华, 刘艳影. 冠心病患者CRP、PCT、SAA水平与冠状动脉粥样硬化程度的相关性分析[J]. 现代诊断与治疗, 2022, 33(2):271-273+290. |
| [8] | Seydel GS, Gunturk I, Akkaya H, et al. The relationship between the new inflammatory markers and disease severity in patients with acute coronary syndrome[J]. Acta Cardiol, 2024, 79(7):778-786. |
| [9] |
Li X, Chen Y, Yuan Q, et al. Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio associated with 28-day all-cause mortality in septic patients with coronary artery disease: A retrospective analysis of MIMIC-IV database[J]. BMC Infect Dis, 2024, 24(1):749.
doi: 10.1186/s12879-024-09516-5 pmid: 39075364 |
| [10] | 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志, 2019, 47(10):766-783. |
| [11] |
Ajoolabady A, Pratico D, Lin L, et al. Inflammation in atherosclerosis: Pathophysiology and mechanisms[J]. Cell Death Dis, 2024, 15(11):817.
doi: 10.1038/s41419-024-07166-8 pmid: 39528464 |
| [12] | 邹谧, 潘静, 周平, 等. 炎症指标对冠状动脉狭窄程度的预测价值[J]. 岭南心血管病杂志, 2023, 29(4):349-353. |
| [13] | 李洋, 刘炳, 董丽, 等. 中性粒细胞与淋巴细胞比值及超敏C反应蛋白与急性冠脉综合征病变程度的相关性研究[J]. 现代医药卫生, 2019, 35(11):1619-1621. |
| [14] | 王忠奇, 李今朝, 吴南. 急性冠脉综合征患者全身免疫炎症指数与冠状动脉病变严重程度的相关性[J]. 临床荟萃, 2024, 39(6):512-517. |
| [15] | Karaca G, Ekmekci A, Kimiaei A, et al. The impact of the neutrophil-to-lymphocyte ratio on in-hospital outcomes in patients with acute ST-segment elevation myocardial infarction[J]. Cureus, 2024, 16(2):e54418. |
| [16] |
de Liyis BG, Ciaves AF, Intizam MH, et al. Hematological biomarkers of troponin, neutrophil-to-lymphocyte ratio, and monocyte-to-lymphocyte ratio serve as effective predictive indicators of high-risk mortality in acute coronary syndrome[J]. Biomedicine (Taipei), 2023, 13(4):32-43.
doi: 10.37796/2211-8039.1425 pmid: 38532835 |
| [17] |
Wang H, Li L, Ma Y. Platelet-to-lymphocyte ratio a potential prognosticator in acute myocardial infarction: A prospective longitudinal study[J]. Clin Cardiol, 2023, 46(6):632-638.
doi: 10.1002/clc.24002 pmid: 37060180 |
| [18] | Carestia A, Godin LC, Jenne CN. Step up to the platelet: Role of platelets in inflammation and infection[J]. Thromb Res, 2023, 231:182-194. |
| [19] |
Siedlinski M, Jozefczuk E, Xu X, et al. White blood cells and blood pressure: A mendelian randomization study[J]. Circulation, 2020, 141(16):1307-1317.
doi: 10.1161/CIRCULATIONAHA.119.045102 pmid: 32148083 |
| [20] | Poller WC, Downey J, Mooslechner AA, et al. Brain motor and fear circuits regulate leukocytes during acute stress[J]. Nature, 2022, 607(7919):578-584. |
| [21] |
Xian H, Liu Y, Rundberg Nilsson A, et al. Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation[J]. Immunity, 2021, 54(7):1463-1477.
doi: 10.1016/j.immuni.2021.05.004 pmid: 34115964 |
| [22] | Ebert T, Anker SD, Ruilope LM, et al. Outcomes with finerenone in patients with chronic kidney disease and type 2 diabetes by baseline insulin resistance[J]. Diabetes Care, 2024, 47(3):362-370. |
| [23] | Keeter WC, Moriarty AK, Galkina EV. Role of neutrophils in type 2 diabetes and associated atherosclerosis[J]. Int J Biochem Cell Biol, 2021, 141:106098. |
| [24] | Zhang X, Kang Z, Yin D, et al. Role of neutrophils in different stages of atherosclerosis[J]. Innate Immun, 2023, 29(6):97-109. |
| [25] | 徐慧, 刘芳. 单核细胞在冠状动脉粥样硬化性心脏病中的研究进展[J]. 岭南心血管病杂志, 2020, 26(5):600-602. |
| [26] |
Orhan AL, Şaylık F, Çiçek V, et al. Evaluating the systemic immune-inflammation index for in-hospital and long-term mortality in elderly non-ST-elevation myocardial infarction patients[J]. Aging Clin Exp Res, 2022, 34(7):1687-1695.
doi: 10.1007/s40520-022-02103-1 pmid: 35275375 |
| [27] |
Hou Y, Si K, Yang J, et al. Association between regulatory T cells and ischemic heart disease: A Mendelian randomization study[J]. J Thorac Dis, 2024, 16(1):564-572.
doi: 10.21037/jtd-23-1790 pmid: 38410592 |
| [28] |
Coenen DM, Heinzmann ACA, Karel MFA, et al. The multifaceted contribution of platelets in the emergence and aftermath of acute cardiovascular events[J]. Atherosclerosis, 2021, 319:132-141.
doi: 10.1016/j.atherosclerosis.2020.12.017 pmid: 33468314 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||