Clinical Focus ›› 2025, Vol. 40 ›› Issue (5): 445-449.doi: 10.3969/j.issn.1004-583X.2025.05.011
Previous Articles Next Articles
Serum level of IL-33 in premature infants with bronchopulmonary dysplasia complicated with pulmonary hypertension and its clinical significance
Wei Jing1, Cui Qingyang1( ), Han Huizhen2, Yan Huili2, Liu Qingsheng2
), Han Huizhen2, Yan Huili2, Liu Qingsheng2
- 1. Department of Neonatology, the First Affiliated Hospital of Xinxiang Medical University, Weihui 453000, China
2. Department of Neonatology, Maternal and Child Health Hospital of Jiaozuo City, Jiaozuo 454001, China
-
Received:2025-02-23Online:2025-05-20Published:2025-05-23 -
Contact:Cui Qingyang E-mail:1282592772@qq.com
CLC Number:
Cite this article
Wei Jing, Cui Qingyang, Han Huizhen, Yan Huili, Liu Qingsheng. Serum level of IL-33 in premature infants with bronchopulmonary dysplasia complicated with pulmonary hypertension and its clinical significance[J]. Clinical Focus, 2025, 40(5): 445-449.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: http://www.lchc.cn/EN/10.3969/j.issn.1004-583X.2025.05.011
| 组别 | 例数 | IL-33(pg/ml) |
|---|---|---|
| 对照组 | 50 | 150.65±15.55 |
| BPD组 | 74 | 389.66±20.45* |
| BPD合并肺动脉高压组 | 56 | 445.56±23.78*# |
| F值 | 45.421 | |
| P值 | <0.001 |
Tab.1 Comparison of serum IL-33 levels among the three groups
| 组别 | 例数 | IL-33(pg/ml) |
|---|---|---|
| 对照组 | 50 | 150.65±15.55 |
| BPD组 | 74 | 389.66±20.45* |
| BPD合并肺动脉高压组 | 56 | 445.56±23.78*# |
| F值 | 45.421 | |
| P值 | <0.001 |
| 项目 | BPD组(n=74) | BPD合并肺动脉高压组(n=56) | t/χ2值 | P值 |
|---|---|---|---|---|
| 母亲妊娠年龄(周岁) | 31.15±4.17 | 30.39±4.51 | 0.993 | 0.322 |
| 母亲妊娠前BMI(kg/m2) | 24.08±4.84 | 24.53±4.37 | 0.547 | 0.585 |
| 剖宫产[例(%)] | 43(58.11) | 40(71.43) | 2.450 | 0.117 |
| 母乳喂养[例(%)] | 68(91.89) | 49(87.50) | 0.683 | 0.408 |
| 妊娠期高血压[例(%)] | 15(20.27) | 12(21.42) | 0.026 | 0.872 |
| 妊娠期糖尿病[例(%)] | 25(33.78) | 24(42.85) | 1.117 | 0.290 |
| 羊水污染[例(%)] | 6(8.11) | 12(21.43) | 4.742 | 0.029 |
| 绒毛膜羊膜炎[例(%)] | 24(32.43) | 32(57.14) | 7.937 | 0.005 |
| 出生胎龄(周) | 29.23±1.90 | 28.67±1.78 | 1.710 | 0.090 |
| 男性[例(%)] | 40(54.05) | 30(53.57) | 0.003 | 0.956 |
| 出生体质量(g) | 1 198.78±313.86 | 1 143.57±350.04 | 0.945 | 0.346 |
| 5 min Apgar评分(分) | 8.37±1.61 | 7.70±1.51 | 2.413 | 0.017 |
| BPD分级[例(%)] | ||||
| Ⅰ~Ⅱ级 Ⅲ级 | 55(74.32) 19(25.68) | 29(51.79) 27(48.21) | 7.082 | 0.008 |
| 呼吸衰竭[例(%)] | 17(22.97) | 24(42.86) | 5.837 | 0.016 |
| 机械通气[例(%)] | 19(25.68) | 30(53.57) | 10.562 | 0.001 |
| 呼吸机相关性肺炎[例(%)] | 5(6.76) | 11(19.64) | 4.904 | 0.027 |
Tab.2 Univariate analysis of BPD combined with pulmonary hypertension in preterm infants
| 项目 | BPD组(n=74) | BPD合并肺动脉高压组(n=56) | t/χ2值 | P值 |
|---|---|---|---|---|
| 母亲妊娠年龄(周岁) | 31.15±4.17 | 30.39±4.51 | 0.993 | 0.322 |
| 母亲妊娠前BMI(kg/m2) | 24.08±4.84 | 24.53±4.37 | 0.547 | 0.585 |
| 剖宫产[例(%)] | 43(58.11) | 40(71.43) | 2.450 | 0.117 |
| 母乳喂养[例(%)] | 68(91.89) | 49(87.50) | 0.683 | 0.408 |
| 妊娠期高血压[例(%)] | 15(20.27) | 12(21.42) | 0.026 | 0.872 |
| 妊娠期糖尿病[例(%)] | 25(33.78) | 24(42.85) | 1.117 | 0.290 |
| 羊水污染[例(%)] | 6(8.11) | 12(21.43) | 4.742 | 0.029 |
| 绒毛膜羊膜炎[例(%)] | 24(32.43) | 32(57.14) | 7.937 | 0.005 |
| 出生胎龄(周) | 29.23±1.90 | 28.67±1.78 | 1.710 | 0.090 |
| 男性[例(%)] | 40(54.05) | 30(53.57) | 0.003 | 0.956 |
| 出生体质量(g) | 1 198.78±313.86 | 1 143.57±350.04 | 0.945 | 0.346 |
| 5 min Apgar评分(分) | 8.37±1.61 | 7.70±1.51 | 2.413 | 0.017 |
| BPD分级[例(%)] | ||||
| Ⅰ~Ⅱ级 Ⅲ级 | 55(74.32) 19(25.68) | 29(51.79) 27(48.21) | 7.082 | 0.008 |
| 呼吸衰竭[例(%)] | 17(22.97) | 24(42.86) | 5.837 | 0.016 |
| 机械通气[例(%)] | 19(25.68) | 30(53.57) | 10.562 | 0.001 |
| 呼吸机相关性肺炎[例(%)] | 5(6.76) | 11(19.64) | 4.904 | 0.027 |
| 指标 | 赋值 |
|---|---|
| 母亲妊娠年龄 | 实际值 |
| 母亲妊娠前BMI | 实际值 |
| 剖宫产 | 无=0,有=1 |
| 母乳喂养 | 无=0,有=1 |
| 妊娠期高血压 | 无=0,有=1 |
| 妊娠期糖尿病 | 无=0,有=1 |
| 羊水污染 | 无=0,有=1 |
| 绒毛膜羊膜炎 | 无=0,有=1 |
| 出生胎龄 | 实际值赋值 |
| 胎儿性别 | 男=0,女=1 |
| 出生体质量 | 实际值 |
| 5 min Apgar评分 | 实际值 |
| BPD分级 | I~II级=0,III级=1 |
| 呼吸衰竭 | 无=0,有=1 |
| 机械通气 | 无=0,有=1 |
| 呼吸机相关性肺炎 | 无=0,有=1 |
| IL-33 | 实际值 |
Tab.3 Variable assignment
| 指标 | 赋值 |
|---|---|
| 母亲妊娠年龄 | 实际值 |
| 母亲妊娠前BMI | 实际值 |
| 剖宫产 | 无=0,有=1 |
| 母乳喂养 | 无=0,有=1 |
| 妊娠期高血压 | 无=0,有=1 |
| 妊娠期糖尿病 | 无=0,有=1 |
| 羊水污染 | 无=0,有=1 |
| 绒毛膜羊膜炎 | 无=0,有=1 |
| 出生胎龄 | 实际值赋值 |
| 胎儿性别 | 男=0,女=1 |
| 出生体质量 | 实际值 |
| 5 min Apgar评分 | 实际值 |
| BPD分级 | I~II级=0,III级=1 |
| 呼吸衰竭 | 无=0,有=1 |
| 机械通气 | 无=0,有=1 |
| 呼吸机相关性肺炎 | 无=0,有=1 |
| IL-33 | 实际值 |
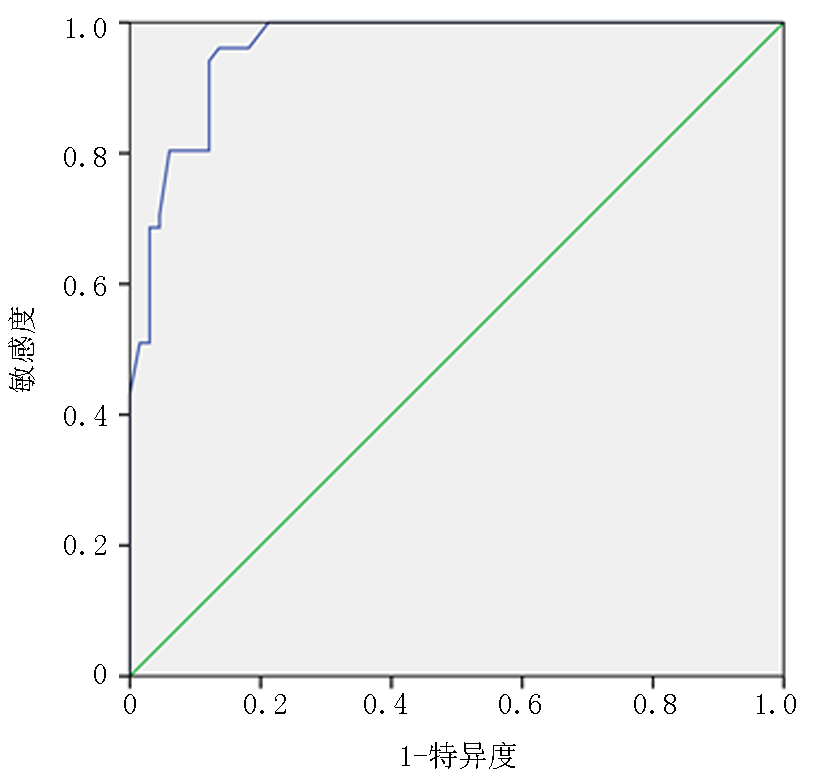
| 因素 | B值 | SE值 | Wald χ2值 | OR值 | P值 | 95%CI |
|---|---|---|---|---|---|---|
| BPD分级(Ⅲ级) | 1.237 | 0.568 | 4.742 | 3.445 | 0.001 | 1.331~6.781 |
| 呼吸机相关性肺炎(有) | 1.169 | 0.889 | 1.728 | 3.218 | 0.001 | 1.452~5.401 |
| IL-33表达水平 | 1.409 | 0.675 | 4.355 | 4.091 | 0.001 | 1.421~10.673 |
Tab.4 Logistic regression analysis of risk factors for BPD combined with pulmonary hypertension in preterm infants
| 因素 | B值 | SE值 | Wald χ2值 | OR值 | P值 | 95%CI |
|---|---|---|---|---|---|---|
| BPD分级(Ⅲ级) | 1.237 | 0.568 | 4.742 | 3.445 | 0.001 | 1.331~6.781 |
| 呼吸机相关性肺炎(有) | 1.169 | 0.889 | 1.728 | 3.218 | 0.001 | 1.452~5.401 |
| IL-33表达水平 | 1.409 | 0.675 | 4.355 | 4.091 | 0.001 | 1.421~10.673 |
| 组别 | 例数 | 肺部感染[例(%)] |
|---|---|---|
| IL-33低表达组 | 64 | 9(14.06) |
| IL-33高表达组 | 66 | 20(30.30) |
| χ2值 | 4.945 | |
| P值 | 0.026 |
Tab.5 Correlation between serum IL-33 level and pulmonary infection in preterm infants with BPD
| 组别 | 例数 | 肺部感染[例(%)] |
|---|---|---|
| IL-33低表达组 | 64 | 9(14.06) |
| IL-33高表达组 | 66 | 20(30.30) |
| χ2值 | 4.945 | |
| P值 | 0.026 |
| [1] | 赵一品, 崔清洋. 超早产儿/超低出生体重儿支气管肺发育不良危险因素分析[J]. 临床荟萃, 2025, 40(1):60-64. |
| [2] | Schmidt AR, Ramamoorthy C. Bronchopulmonary dysplasia[J]. Paediatr Anaesth, 2022, 32(2):174-180. |
| [3] | 束辉玲. 急性呼吸窘迫综合征早产儿发生支气管肺发育不良的危险因素分析[J]. 中国医药科学, 2023, 13(14):90-93. |
| [4] |
Zhou Y, Xu Z, Liu Z. Role of IL-33-ST2 pathway in regulating inflammation: Current evidence and future perspectives[J]. J Transl Med, 2023, 21(1):902.
doi: 10.1186/s12967-023-04782-4 pmid: 38082335 |
| [5] | 曹婧可, 范浩钦, 肖云彬, 等. 极早产儿支气管肺发育不良相关肺动脉高压临床预测模型的建立和效能检验[J]. 中华儿科杂志, 2024, 62(2):129-137. |
| [6] | Higgins RD, Jobe AH, Koso-Thomas M, et al. Bronchopulmonary dysplasia: Executive summary of a workshop[J]. J Pediatr, 2018, 197:300-308. |
| [7] | 中华医学会儿科学分会新生儿学组, 《中华儿科杂志》编辑委员会. 新生儿肺动脉高压诊治专家共识[J]. 中华儿科杂志, 2017, 55(3):163-168. |
| [8] | 中华医学会儿科学分会新生儿学组, 中华儿科杂志编辑委员会. 早产儿支气管肺发育不良临床管理专家共识[J]. 中华儿科杂志, 2020, 58(5):358-365. |
| [9] | Miller AN, Shepherd EG, El-Ferzli G, et al. Multidisciplinary bronchopulmonary dysplasia care[J]. Expert Rev Respir Med, 2023, 17(11):989-1002. |
| [10] | Carregã M, Sousa P, Rocha G, et al. Respiratory and non-respiratory outcomes of bronchopulmonary dysplasia in adolescents: A systematic review[J]. Early Hum Dev, 2023, 180:105756. |
| [11] |
Al-Ghanem G, Shah P, Thomas S, et al. Bronchopulmonary dysplasia and pulmonary hypertension: A meta-analysis[J]. J Perinatol, 2017, 37(4):414-419.
doi: 10.1038/jp.2016.250 pmid: 28079864 |
| [12] | Levy PT, Levin J, Leeman KT, et al. Diagnosis and management of pulmonary hypertension in infants with bronchopulmonary dysplasia[J]. Semin Fetal Neonatal Med, 2022, 27(4):101351. |
| [13] | Gentle SJ, Travers CP, Nakhmani A, et al. Intermittent hypoxemia and bronchopulmonary dysplasia with pulmonary hypertension in preterm infants[J]. Am J Respir Crit Care Med, 2023, 207(7):899-907. |
| [14] | 贾毅, 张东平, 郑玲芳, 等. 早产儿支气管肺发育不良的影响因素及血清IL-33和sST2的预测价值[J]. 中国优生与遗传杂志, 2020, 28(11):1384-1387. |
| [15] | 刘杰, 沙宇惠, 高阳, 等. IL-33通过活化巨噬细胞NF-κB信号通路参与低氧性肺动脉高压的发生发展[J]. 微生物学免疫学进展, 2018, 46(4):26-34. |
| [16] | Indralingam CS, Gutierrez-Gonzalez AK, Johns SC, et al. IL-33/ST2 receptor-dependent signaling in the development of pulmonary hypertension in sugen/hypoxia mice[J]. Physiol Rep, 2022, 10(3):e15185. |
| [17] | 陈春, 黄鹏, 林冰纯, 等. 早产儿支气管肺发育不良伴肺动脉高压的高危因素与转归[J]. 中华儿科杂志, 2020, 58(9):747-752. |
| [18] | 刘选成, 谷名晓, 单若冰, 等. 极低出生体重儿支气管肺发育不良并发肺动脉高压的影响因素[J]. 山东医药, 2024, 64(4):77-80. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||