Clinical Focus ›› 2025, Vol. 40 ›› Issue (6): 541-546.doi: 10.3969/j.issn.1004-583X.2025.06.011
Previous Articles Next Articles
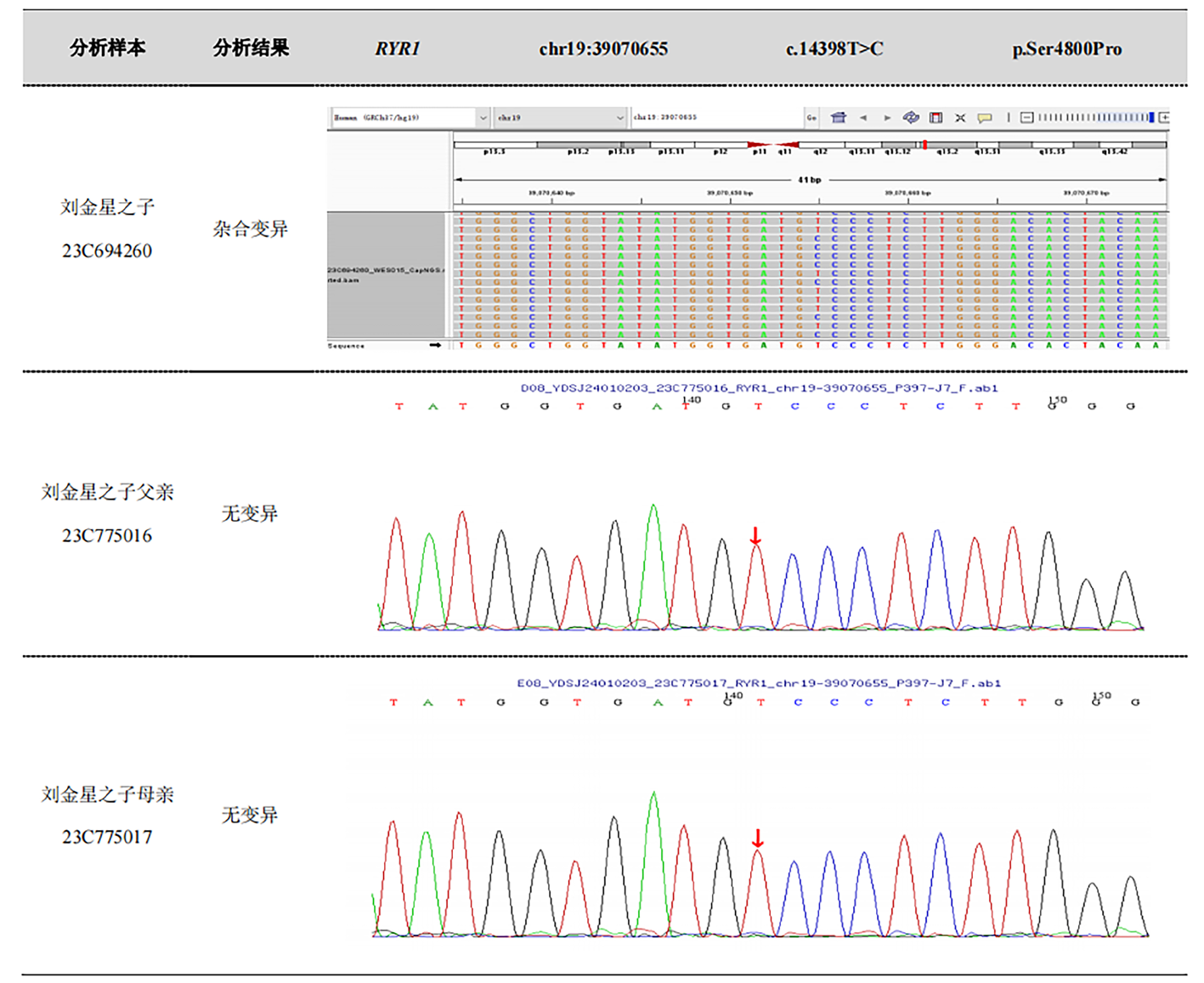
Neonatal ryanodine receptor type 1-related myopathies: A case report and literature review
Wang Sihan1, Li Xianghong2, Li Liangliang2, Xi Hongmin2, Yang Ping2, Ma Lili2, Yin Xiangyun2( )
)
- 1. Qingdao Medical College, Qingdao University, Qingdao 266100, China
2. Department of Neonatology, the Affiliated Hospital of Qingdao University, Qingdao 266400, China
-
Received:2025-04-22Online:2025-06-20Published:2025-07-01 -
Contact:Yin Xiangyun E-mail:yinxiangyun415@sina.com
CLC Number:
Cite this article
Wang Sihan, Li Xianghong, Li Liangliang, Xi Hongmin, Yang Ping, Ma Lili, Yin Xiangyun. Neonatal ryanodine receptor type 1-related myopathies: A case report and literature review[J]. Clinical Focus, 2025, 40(6): 541-546.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: http://www.lchc.cn/EN/10.3969/j.issn.1004-583X.2025.06.011
| [1] | Ogasawara M, Nishino I. A review of major causative genes in congenital myopathies[J]. J Hum Genet, 2023, 68(3):215-225. |
| [2] |
Zhang Y, Yan H, Liu J, et al. Clinical and genetic features of infancy-onset congenital myopathies from a Chinese paediatric centre[J]. BMC Pediatr, 2022, 22(1):65.
doi: 10.1186/s12887-021-03024-0 pmid: 35081925 |
| [3] |
Witherspoon JW, Vuillerot C, Vasavada RP, et al. Motor function performance in individuals with RYR1-related myopathies[J]. Muscle Nerve, 2019, 60(1):80-87.
doi: 10.1002/mus.26491 pmid: 31004442 |
| [4] | 徐海峰, 王尚玉, 应国环, 等. 先天性肌病的临床、病理特征及分子遗传学分析八例[J]. 现代医学, 2024, 52(4):627-634. |
| [5] | Sarkozy A, Sa M, Ridout D, et al. Long-term natural history of pediatric dominant and recessive RYR1-related myopathy[J]. Neurology, 2023, 101(15):e1495-e1508. |
| [6] | Murayama T, Kurebayashi N, Ishida R, et al. Drug development for the treatment of RyR1-related skeletal muscle diseases[J]. Curr Opin Pharmacol, 2023, 69:102356. |
| [7] | Campiglio M, Dyrda A, Tuinte WE, et al. Ca(V)1.1 calcium channel signaling complexes in excitation-contraction coupling: Insights from channelopathies[J]. Handb Exp Pharmacol, 2023,279:3-39. |
| [8] |
Lawal TA, Todd JJ, Meilleur KG. Ryanodine receptor 1-related myopathies: Diagnostic and therapeutic approaches[J]. Neurotherapeutics, 2018, 15(4):885-899.
doi: 10.1007/s13311-018-00677-1 pmid: 30406384 |
| [9] |
Jungbluth H, Treves S, Zorzato F, et al. Congenital myopathies: Disorders of excitation-contraction coupling and muscle contraction[J]. Nat Rev Neurol, 2018, 14(3):151-167.
doi: 10.1038/nrneurol.2017.191 pmid: 29391587 |
| [10] | Todd JJ, Razaqyar MS, Witherspoon JW, et al. Novel variants in individuals with RYR1-related congenital myopathies: Genetic, laboratory, and clinical findings[J]. Front Neurol, 2018, 9:118. |
| [11] | 吴士文, 马维娅, 苏慧, 等. 中央轴空病1例[J]. 武警医学, 2007, 18(11):862. |
| [12] | 张天可, 叶静怡, 李克秋, 等. 1个中央轴空病家系RYR1基因的突变分析[J]. 国际遗传学杂志, 2015, 38(2):59-63. |
| [13] | 宋金涛. 中央轴空病1例报告[J]. 中国临床医学, 2019, 26(5):794-796. |
| [14] | 笪宇威, 王敏, 卢岩, 等. 常染色体显性遗传性中央轴空病的临床表现和病理特点[J]. 卒中与神经疾病, 2009, 16(6):335-337. |
| [15] | 董孝云, 郑璇, 林法涛, 等. 一例新生儿中央轴空病的临床特点及家系基因变异分析[J]. 中华医学遗传学杂志, 2022, 39(6):607-610. |
| [16] | Helbling DC, Mendoza D, McCarrier J, et al. Severe neonatal RYR1 myopathy with pathological features of congenital muscular dystrophy[J]. J Neuropathol Exp Neurol, 2019, 78(3):283-287. |
| [17] |
Wu S, Ibarra MC, Malicdan MC, et al. Central core disease is due to RYR1 mutations in more than 90% of patients[J]. Brain, 2006, 129(Pt 6):1470-1480.
pmid: 16621918 |
| [18] |
Quinlivan RM, Muller CR, Davis M, et al. Central core disease: Clinical, pathological, and genetic features[J]. Arch Dis Child, 2003, 88(12):1051-1055.
pmid: 14670767 |
| [19] |
Jungbluth H, Müller CR, Halliger-Keller B, et al. Autosomal recessive inheritance of RYR1 mutations in a congenital myopathy with cores[J]. Neurology, 2002, 59(2):284-287.
pmid: 12136074 |
| [20] |
Monnier N, Romero NB, Lerale J, et al. Familial and sporadic forms of central core disease are associated with mutations in the C-terminal domain of the skeletal muscle ryanodine receptor[J]. Hum Mol Genet, 2001, 10(22):2581-2592.
pmid: 11709545 |
| [21] | Baker EK, Al Gharaibeh FN, Bove K, et al. A novel RYR1 variant in an infant with a unique fetal presentation of central core disease[J]. Am J Med Genet A, 2023, 191(6):1646-1651. |
| [22] |
João PM, Alves PB, Ana G, et al. Congenital myopathies in adults: A diagnosis not to overlook[J]. Acta Neurol Scand, 2022, 146(2):152-159.
doi: 10.1111/ane.13632 pmid: 35548885 |
| [23] | Gaspar BL. A novel homozygous variant of RYR1 p.Ala3072Asp in a neonate with dusty core disease: A new entity with clinicopathological implications[J]. Neuropathology, 2020, 40(4):367-372. |
| [24] |
Hayakawa I, Abe Y, Ono H, et al. Severe congenital RYR1-associated myopathy complicated with atrial tachycardia and sinus node dysfunction: A case report[J]. Ital J Pediatr, 2019, 45(1):165.
doi: 10.1186/s13052-019-0756-1 pmid: 31856875 |
| [25] | Marks S, Ruitenbeek Ev, Fallon P, et al. Parental mosaicism in RYR1-related central core disease[J]. Neuromuscul Disord, 2018, 28(5):422-426. |
| [26] | Laforgia N, Capozza M, De Cosmo L, et al. A rare case of severe congenital RYR1-associated myopathy[J]. Case Rep Genet, 2018, 2018:6184185. |
| [27] | Brackmann F, Türk M, Gratzki N, et al. Compound heterozygous RYR1 mutations in a preterm with arthrogryposis multiplex congenita and prenatal CNS bleeding[J]. Neuromuscul Disord, 2018, 28(1):54-58. |
| [28] |
Rocha J, Taipa R, Pires MM, et al. Ryanodine myopathies without central cores-clinical, histopathologic, and genetic description of three cases[J]. Pediatr Neurol, 2014, 51(2):275-278.
doi: 10.1016/j.pediatrneurol.2014.04.024 pmid: 24950660 |
| [29] | Pandey R, Chandratre S, Roberts A, et al. Central core myopathy with RYR1 mutation masks 5q spinal muscular atrophy[J]. Eur J Paediatr Neurol, 2010, 15(1):70-73. |
| [30] | Hernandez-Lain A, Husson I, Monnier N, et al. De novo RYR1 heterozygous mutation (I4898T) causing lethal core-rod myopathy in twins[J]. Eur J Med Genet, 2010, 54(1):29-33. |
| [31] |
Erendzhinova E, Robinson CA, Lowry NJ, et al. Familial RYR 1 mutation associated with mild and severe central core disease[J]. Can J Neurol Sci, 2010, 37(4):528-531.
pmid: 20724266 |
| [32] |
Nicole M, Isabelle M, Julien F, et al. Null mutations causing depletion of the type 1 ryanodine receptor (RYR1) are commonly associated with recessive structural congenital myopathies with cores[J]. Hum Mutat, 2008, 29(5):670-678.
doi: 10.1002/humu.20696 pmid: 18253926 |
| [33] | Jungbluth H, Zhou H, Sewry CA, et al. Centronuclear myopathy due to a de novo dominant mutation in the skeletal muscle ryanodine receptor (RYR1) gene[J]. Neuromuscul Disord, 2007, 17(4):338-345. |
| [34] |
Jungbluth H, Zhou H, Hartley L, et al. Minicore myopathy with ophthalmoplegia caused by mutations in the ryanodine receptor type 1 gene[J]. Neurology, 2005, 65(12):1930-1935.
pmid: 16380615 |
| [35] |
Beatriz RN, Nicole M, Louis V, et al. Dominant and recessive central core disease associated with RYR1 mutations and fetal akinesia[J]. Brain, 2003, 126(Pt 11):2341-2349.
pmid: 12937085 |
| [36] | Zhao XY, Liu F, Wu YY, et al. A call for increased focus on fractures in congenital myopathy infants[J]. Indian J Pediatr, 2024, 91(1):94. |
| [37] | Illingworth MA, Main M, Pitt M, et al. RYR1-related congenital myopathy with fatigable weakness, responding to pyridostigimine[J]. Neuromuscul Disord, 2014, 24(8):707-712. |
| [38] | Zecevic N, Arsenijevic V, Manolakos E, et al. New compound heterozygous splice site mutations of the skeletal muscle ryanodine receptor (RYR1) gene manifest fetal akinesia: A linkage with congenital myopathies[J]. Mol Syndromol, 2020, 11(2):104-109. |
| [39] | Sewry CA, Müller C, Davis M, et al. The spectrum of pathology in central core disease[J]. Neuromuscul Disord, 2002, 12(10):930-938. |
| [40] | Witherspoon JW, Meilleur KG. Review of RyR1 pathway and associated pathomechanisms[J]. Acta Neuropathol Commun, 2016, 4(1):121. |
| [41] | Wu Y, Hamilton SL. Functional interactions of cytoplasmic domains of the skeletal muscle Ca2+ release channel[J]. Trends Cardiovasc Med, 1998, 8(7):312-319. |
| [42] | Treves S, Anderson AA, Ducreux S, et al. Ryanodine receptor 1 mutations, dysregulation of calcium homeostasis and neuromuscular disorders[J]. Neuromuscul Disord, 2005, 15(9-10):577-587. |
| [43] |
Kushnir A, Todd JJ, Witherspoon JW, et al. Intracellular calcium leak as a therapeutic target for RYR1-related myopathies[J]. Acta Neuropathol, 2020, 139(6):1089-1104.
doi: 10.1007/s00401-020-02150-w pmid: 32236737 |
| [44] | Maggi L, Scoto M, Cirak S, et al. Congenital myopathies--clinical features and frequency of individual subtypes diagnosed over a 5-year period in the United Kingdom[J]. Neuromuscul Disord, 2013, 23(3):195-205. |
| [45] | Mary P, Servais L, Vialle R. Neuromuscular diseases: Diagnosis and management[J]. Orthop Traumatol Surg Res, 2018, 104(1s):S89-s95. |
| [46] |
Colombo I, Scoto M, Manzur AY, et al. Congenital myopathies: Natural history of a large pediatric cohort[J]. Neurology, 2015, 84(1):28-35.
doi: 10.1212/WNL.0000000000001110 pmid: 25428687 |
| [47] |
Iodice P, Boncompagni S, Pietrangelo L, et al. Functional electrical stimulation: A possible strategy to improve muscle function in central core disease?[J]. Front Neurol, 2019, 10:479.
doi: 10.3389/fneur.2019.00479 pmid: 31191425 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||