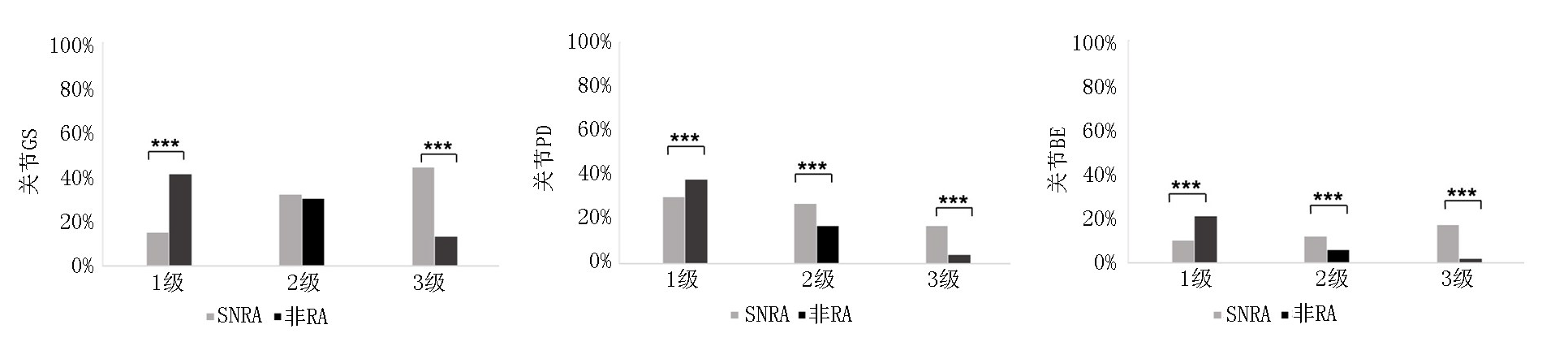
Clinical Focus ›› 2025, Vol. 40 ›› Issue (8): 705-710.doi: 10.3969/j.issn.1004-583X.2025.08.006
Previous Articles Next Articles
Role of musculoskeletal ultrasound in the early diagnosis of seronegative rheumatoid arthritis
Shen Xuejiao, Wang Ting, Wang Yuan, Li Yan, Wei Jiaqi( )
)
- Ultrasound Medical Center, the Second Hospital, Lanzhou University, Lanzhou 730030, China
-
Received:2025-07-01Online:2025-08-20Published:2025-09-05 -
Contact:Wei Jiaqi E-mail:15293191866@163.com
CLC Number:
Cite this article
Shen Xuejiao, Wang Ting, Wang Yuan, Li Yan, Wei Jiaqi. Role of musculoskeletal ultrasound in the early diagnosis of seronegative rheumatoid arthritis[J]. Clinical Focus, 2025, 40(8): 705-710.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.lchc.cn/EN/10.3969/j.issn.1004-583X.2025.08.006
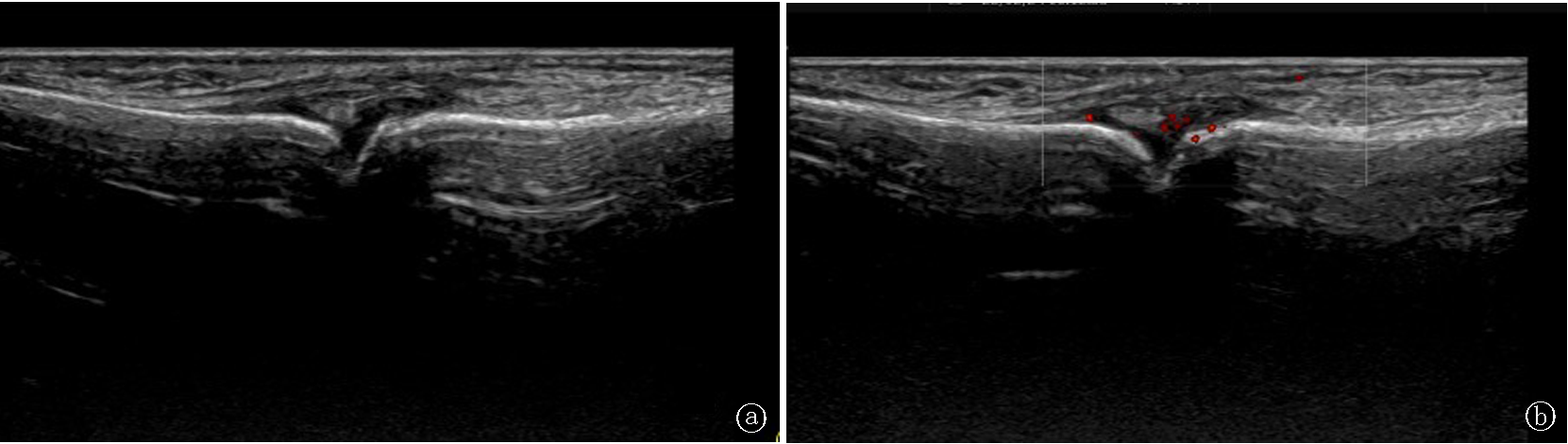
Fig.1 Synovitis of the finger joints a. GS shows grade 2 synovial hyperplasia of the finger joint;b.PD shows blood flow in the grade 2 hyperplastic synovium
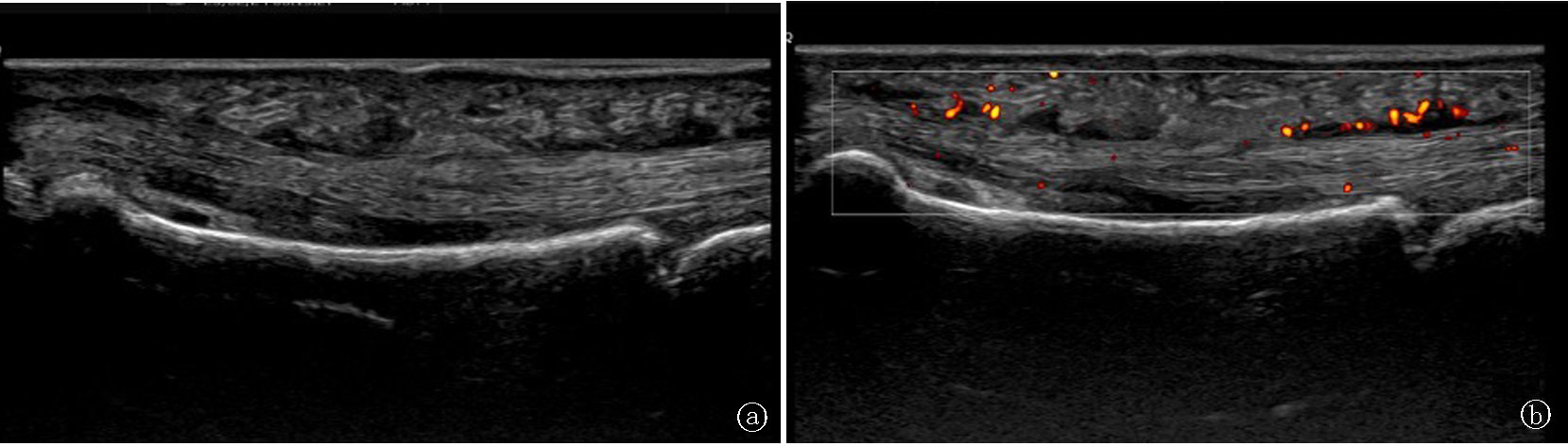
Fig.2 Tenosynovitis of the finger flexor tendons a.GS shows extensive dilation of the flexor tendon sheath (grade 3);b. PD shows blood flow in grade 2 tenosynovitis
| 项目 | SNRA组(n=45) | 非RA组(n=67) | 统计值 | P值 |
|---|---|---|---|---|
| 年龄(岁) | 53.17±13.21 | 49.88±11.34 | t=-1.740 | 0.120 |
| 男性[例(%)] | 8(17.8) | 24(35.8) | χ2=-2.02 | 0.090 |
| 病程(月) | 12.11±16.12 | 10.92±7.67 | t=-2.410 | 0.070 |
| CRP(μg/L) | 51.04±45.35 | 17.33±21.30 | t=-5.480 | <0.01 |
| ESR(mm/h) | 46.38±34.30 | 15.03±15.47 | t=-5.560 | <0.01 |
| 发病部位[例(%)] | ||||
| 腕关节 | 65(72.2) | 82(61.2) | χ2=1.090 | 0.300 |
| MCP1-5 | 143(31.8) | 164(24.5) | χ2=3.260 | 0.160 |
| PIP1-5 | 80(17.8) | 142(21.2) | χ2=0.280 | 0.540 |
Tab.1 Comparison of clinical data and site of onset between the two groups
| 项目 | SNRA组(n=45) | 非RA组(n=67) | 统计值 | P值 |
|---|---|---|---|---|
| 年龄(岁) | 53.17±13.21 | 49.88±11.34 | t=-1.740 | 0.120 |
| 男性[例(%)] | 8(17.8) | 24(35.8) | χ2=-2.02 | 0.090 |
| 病程(月) | 12.11±16.12 | 10.92±7.67 | t=-2.410 | 0.070 |
| CRP(μg/L) | 51.04±45.35 | 17.33±21.30 | t=-5.480 | <0.01 |
| ESR(mm/h) | 46.38±34.30 | 15.03±15.47 | t=-5.560 | <0.01 |
| 发病部位[例(%)] | ||||
| 腕关节 | 65(72.2) | 82(61.2) | χ2=1.090 | 0.300 |
| MCP1-5 | 143(31.8) | 164(24.5) | χ2=3.260 | 0.160 |
| PIP1-5 | 80(17.8) | 142(21.2) | χ2=0.280 | 0.540 |
| 组别 | 例数 | 关节 | 肌腱 | 关节病变 | 肌腱病变 | BE | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| GS1 | PD1 | BE评分 | GS2 | PD2 | ||||||
| SNRA组 | 45 | 16.20±12.23 | 12.82±9.24 | 1.60±1.60 | 8.82±6.55 | 10.13±8.01 | 356(36.0) | 252(23.3) | 48(4.8) | |
| 非RA组 | 67 | 7.40±5.68 | 5.49±5.04 | 1.18±1.95 | 6.92±5.94 | 6.97±6.09 | 297(20.1) | 459(28.5) | 56(3.8) | |
| 统计值 | t=-4.790 | t=-5.237 | t=-2.083 | t=-1.616 | t=-2.082 | χ2=-3.914 | χ2=-1.283 | χ2=-2.217 | ||
| P值 | <0.001 | <0.001 | 0.037 | 0.106 | 0.037 | <0.001 | 0.200 | 0.027 | ||
Tab.2 Comparison of ultrasound scoring indicators between the two groups
| 组别 | 例数 | 关节 | 肌腱 | 关节病变 | 肌腱病变 | BE | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| GS1 | PD1 | BE评分 | GS2 | PD2 | ||||||
| SNRA组 | 45 | 16.20±12.23 | 12.82±9.24 | 1.60±1.60 | 8.82±6.55 | 10.13±8.01 | 356(36.0) | 252(23.3) | 48(4.8) | |
| 非RA组 | 67 | 7.40±5.68 | 5.49±5.04 | 1.18±1.95 | 6.92±5.94 | 6.97±6.09 | 297(20.1) | 459(28.5) | 56(3.8) | |
| 统计值 | t=-4.790 | t=-5.237 | t=-2.083 | t=-1.616 | t=-2.082 | χ2=-3.914 | χ2=-1.283 | χ2=-2.217 | ||
| P值 | <0.001 | <0.001 | 0.037 | 0.106 | 0.037 | <0.001 | 0.200 | 0.027 | ||
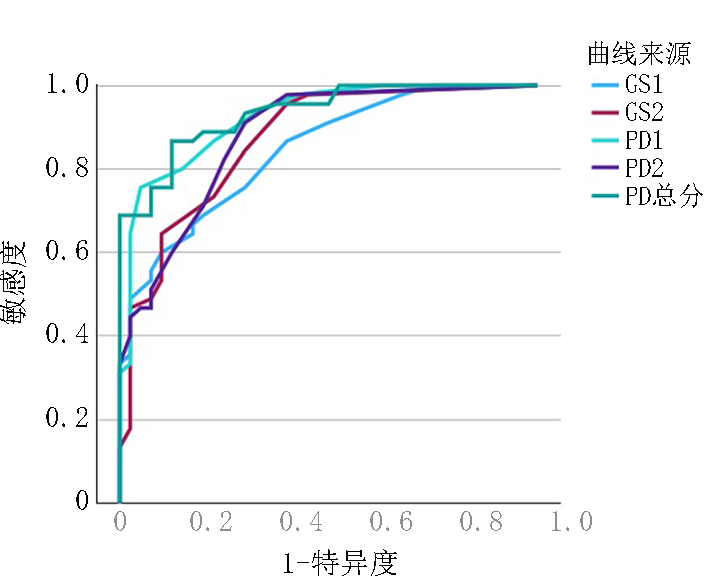
| GS1 | PD1 | BE分级 | GS2 | PD2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r值 | P值 | r值 | P值 | r值 | P值 | r值 | P值 | r值 | P值 | |||||
| CRP | 0.366 | 0.013 | 0.444 | 0.002 | 0.539 | 0.003 | 0.732 | <0.01 | 0.772 | <0.01 | ||||
| ESR | 0.306 | 0.041 | 0.384 | 0.009 | 0.290 | 0.127 | 0.532 | <0.01 | 0.538 | <0.01 | ||||
| 病程 | -0.104 | 0.497 | -0.103 | 0.502 | -0.063 | 0.745 | -0.161 | 0.290 | -0.055 | 0.721 | ||||
Tab.3 Correlation analysis of ultrasound indicators and clinical data in the SNRA group
| GS1 | PD1 | BE分级 | GS2 | PD2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r值 | P值 | r值 | P值 | r值 | P值 | r值 | P值 | r值 | P值 | |||||
| CRP | 0.366 | 0.013 | 0.444 | 0.002 | 0.539 | 0.003 | 0.732 | <0.01 | 0.772 | <0.01 | ||||
| ESR | 0.306 | 0.041 | 0.384 | 0.009 | 0.290 | 0.127 | 0.532 | <0.01 | 0.538 | <0.01 | ||||
| 病程 | -0.104 | 0.497 | -0.103 | 0.502 | -0.063 | 0.745 | -0.161 | 0.290 | -0.055 | 0.721 | ||||
| [1] | Pratt AG, Isaacs JD. Seronegative rheumatoid arthritis: Pathogenetic and therapeutic aspects[J]. BEST PRACT RES CL RH, 2014, 28 (4): 651-659. |
| [2] | 姜楠, 田新平, 曾小峰. 提高规范诊疗水平改善我国类风湿关节炎患者预后[J]. 中华内科杂志, 2024, 63(11):1049-1051. |
| [3] |
Funovits J, Aletaha D, Bykerk V, et al. The 2010 American college of Rheumatology/European League Against Rheumatism classifcation criteria for rheumatoid arthritis: Methodological report phase I[J]. Ann Rheum Dis, 2010, 69(9): 1589-1595.
doi: 10.1136/ard.2010.130310 pmid: 20699242 |
| [4] | Terslev L, Naredo E, Aegerter P, et al. Scoring ultrasound synovitis in rheumatoid arthritis: A EULAR-OMERACT ultrasound taskforce-Part 2: Reliability and application to multiple joints of a standardised consensus-based scoring system[J]. RMD Open, 2017, 3(1): e000427. |
| [5] |
Naredo E, D'Agostino MA, Wakefield RJ, et al. Reliability of a consensus-based ultrasound score for tenosynovitis in rheumatoid arthritis[J]. Ann Rheum Dis, 2013, 72(8):1328-1334.
doi: 10.1136/annrheumdis-2012-202092 pmid: 22984169 |
| [6] |
Ravindran V, Rachapalli S. An overview of commonly used radiographic scoring methods in rheumatoid arthritis clinical trials[J]. Clin Rheumatol, 2011, 30(1): 1-6.
doi: 10.1007/s10067-010-1554-8 pmid: 20730549 |
| [7] |
Courvoisier DS, Chatzidionysiou K, Mongin D, et al. The impact of seropositivity on the effectiveness of biologic anti-rheumatic agents: Results from a coll aboration of 16 registries[J]. Rheumatology, 2021, 60(2):820-828.
doi: 10.1093/rheumatology/keaa393 pmid: 32810263 |
| [8] |
Pertsinidou E, Saevarsdottir S, Manivel VA, et al. In early rheumatoid arthritis, anticitrullinated peptide antibodies associate with low number of affected joints and rheumatoid factor associates with systemic inflammation[J]. ANN RHEUM DIS, 2024, 83 (3): 277-287.
doi: 10.1136/ard-2023-224728 pmid: 38049984 |
| [9] |
Gadeholt O, Hausotter K, Eberle H, et al. Differing X-ray patterns in seronegative and seropositive rheumatoid arthritis[J]. Clin Rheumatol, 2019, 38(9): 2403-2410.
doi: 10.1007/s10067-019-04602-5 pmid: 31123977 |
| [10] | Englund M, Glersen M, Vistnes M, et al. Biomarkers for erosive vs non-erosive hand osteoarthritis: The nor-hand cohort[J]. OSTEOARTHR CARTILAGE, 2024, 32(2):S87-S87. |
| [11] | Sahbudin I, Singh R, De Pablo P, et al. The value of ultrasound-defined tenosynovitis and synovitis in the prediction of persistent arthritis[J]. Rheumatology (Oxford), 2023, 62 (3): 1057-1068. |
| [12] |
Wang J, Wang M, Qi Q, et al. High-frequency ultrasound in patients with seronegative rheumatoid arthritis[J]. Sci Rep, 2022, 12 (1): 21372.
doi: 10.1038/s41598-022-25958-w pmid: 36494477 |
| [13] | Cen Y, He D, Wang P, et al. Contribution of musculoskeletal ultrasound in the diagnosis of seronegative rheumatoid arthritis[J]. J Ultrasound Med, 2024, 43 (10): 1929-1936. |
| [14] |
Xu J, Gong Y, Yang K, et al. A cohort study of ultrasonic semi-quantitative scoring for the diagnosis of serology-negative rheumatoid arthritis[J]. Arch Rheumatol, 2024, 39 (4): 579-587.
doi: 10.46497/ArchRheumatol.2024.10788 pmid: 40060128 |
| [15] |
van den Bosch MHJ, van Lent PLEM, et al. Identifying effector molecules, cells, and cytokines of innate immunity in OA[J]. OSTEOARTHR CARTILAGE, 2020, 28(5): 532-543.
doi: S1063-4584(20)30050-9 pmid: 32044352 |
| [16] | Sunk IG, Amoyo-Minar L, Niederreiter B, et al. Dorso-ventral osteophytes of interphalangeal joints correlate with cartilage damage and synovial inflammation in hand osteoarthritis: A histological/radiographical study[J]. Arthritis Res Ther, 2022, 24 (1): 226. |
| [17] |
Tang Y, Yang Y, Xiang X, et al. Power doppler ultrasound evaluation of peripheral joint, entheses, tendon, and bursa abnormalities in psoriatic patients: A clinical study[J]. J Rheumatol, 2018, 45 (6): 811-817.
doi: 10.3899/jrheum.170765 pmid: 29657139 |
| [18] | Nieuwenhuis WP, Krabben A, Stomp W, et al. Evaluation of magnetic resonance imaging-detected tenosynovitis in the hand and wrist in early arthritis[J]. Arthritis Rheumatol, 2015, 67(4):869-876. |
| [19] |
Hammer HB, Kvien TK, Terslev L. Tenosynovitis in rheumatoid arthritis patients on biologic treatment: Involvement and sensitivity to change compared to joint inflammation[J]. Clin Exp Rheumatol, 2017, 35(6):959-965.
pmid: 28516887 |
| [20] | Nordberg LB, Lillegraven S, Lie E. Patients with seronegative RA have more inflammatory activity compared with patients with seropositive RA in an inception cohort of DMARD-naive patients classified according to the 2010 ACR/EULAR criteria[J]. Ann Rheum Dis, 2016, 76(2):341-345. |
| [21] | Ruta S, Sanchez Prado E, Salvatori F, et al. Ultrasound tenosynovitis: A differential feature of patients with seronegative rheumatoid arthritis[J]. Reumatol Clin (Engl Ed), 2023, 19 (2): 63-66. |
| [1] | Zhao Hui, Zhang Pengwei, Zhang Jian, Huang Wenhui, Li Xiaoli, Ma Zhigang, Jin Fang, Tian Limin. IgA-dominant infection-related glomerulonephritis with oxalate deposition: A case report and literature review [J]. Clinical Focus, 2025, 40(2): 162-167. |
| [2] | Hu Zelin, Wu Meixuan, Mei Jia, Meng Shujing, Zhang Qiang, Qin Dianju. Summary of evidence for exercise interventions in patients with knee osteoarthritis [J]. Clinical Focus, 2024, 39(5): 396-400. |
| [3] | Li Huiting, Meng Jinghong, Gu Guang, Chen Haiying, Wang Junxiang. Clinical characteristics of ankylosing spondylitis with hip involvement [J]. Clinical Focus, 2021, 36(6): 500-503. |
| [4] | Shi Bohan, Huang Chunmeng, Zhu Yan, Chen Zhu, Li Kunpeng, Luo Yun, Xiao Zhongxin, Tang Yanfu, Xu Qian, Xu Yan. Shortterm clinical efficacy of Kinesio Taping on walking ability of patients with knee osteoarthritis [J]. Clinical Focus, 2020, 35(12): 1111-1115. |
| [5] | Li Hongchao, Song Hui. Inflammatory arthropathy and osteoporosis [J]. Clinical Focus, 2019, 34(4): 312-315. |
| [6] | Sun Chaoa, Peng Chenxinga, Qi Xuana, Guo Huifanga, Lei Lingyana, Zhang Jingyub. Application value of high frequency ultrasound in hemophiliac arthropathy [J]. Clinical Focus, 2018, 33(6): 502-505. |
| [7] | Qi Xuan, Sun Chao, Tian Yu, Ding Meng. Evaluation of curative effect of KunXian capsule on knee osteoarthritis by high frequency ultrasound [J]. Clinical Focus, 2018, 33(4): 306-310. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||