Clinical Focus ›› 2025, Vol. 40 ›› Issue (8): 698-704.doi: 10.3969/j.issn.1004-583X.2025.08.005
Previous Articles Next Articles
Analysis of prognostic risk factors and predictive value in patients with bloodstream infection complicated with sepsis
Zhuang Huicui1, Guo Hao2( ), Li Xian2, Cui Dongsheng2
), Li Xian2, Cui Dongsheng2
- 1. Department of Critical Care Medicine, Jiaozhou Central Hospital of Qingdao, Qingdao 266000, China
2. Department of Critical Care Medicine, Handan Central Hospital, Handan 056001, China
-
Received:2025-04-24Online:2025-08-20Published:2025-09-05 -
Contact:Guo Hao E-mail:guohao1974@163.com
CLC Number:
Cite this article
Zhuang Huicui, Guo Hao, Li Xian, Cui Dongsheng. Analysis of prognostic risk factors and predictive value in patients with bloodstream infection complicated with sepsis[J]. Clinical Focus, 2025, 40(8): 698-704.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.lchc.cn/EN/10.3969/j.issn.1004-583X.2025.08.005
| 项目 | 例数(例) | 百分比(%) |
|---|---|---|
| 性别 | ||
| 男 | 92 | 56.8 |
| 女 | 70 | 43.2 |
| 年龄(岁) | ||
| <60 | 45 | 27.8 |
| 60~74 | 79 | 48.8 |
| ≥75 | 38 | 23.4 |
| 28 d预后情况 | ||
| 死亡 | 91 | 56.2 |
| 存活 | 71 | 43.8 |
Tab.1 General information of sepsis patients with BSI (n=162)
| 项目 | 例数(例) | 百分比(%) |
|---|---|---|
| 性别 | ||
| 男 | 92 | 56.8 |
| 女 | 70 | 43.2 |
| 年龄(岁) | ||
| <60 | 45 | 27.8 |
| 60~74 | 79 | 48.8 |
| ≥75 | 38 | 23.4 |
| 28 d预后情况 | ||
| 死亡 | 91 | 56.2 |
| 存活 | 71 | 43.8 |
| 组别 | 例数 | 性别[例(%)] | 年龄 (岁) | 社区获得性 [例(%)] | 非ICU医院 获得性 [例(%)] | ICU获得性 [例(%)] | 评分(分) | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | SOFA 评分 | APACHEⅡ 评分 | mNUTRIC 评分 | SIC 评分 | ||||||||||||||||||||||||||
| 死亡组 | 91 | 55(60.4) | 36(39.6) | 71(63, 76) | 45(49.5) | 19(20.9) | 27(29.7) | 13(11, 15) | 25(20, 31) | 7(6, 8) | 4(3, 6) | ||||||||||||||||||||
| 存活组 | 71 | 37(52.1) | 34(47.9) | 63(50, 71) | 50(70.4) | 11(15.5) | 10(14.1) | 8(6, 11) | 18(14, 22) | 5(3, 6) | 4(3, 5) | ||||||||||||||||||||
| t/Z/χ2值 | 1.127 | -3.384 | 7.233 | 0.767 | 5.497 | -7.157 | -6.523 | -5.700 | -2.724 | ||||||||||||||||||||||
| P值 | 0.288 | 0.001 | 0.007 | 0.381 | 0.019 | 0.000 | 0.000 | 0.000 | 0.006 | ||||||||||||||||||||||
| 组别 | 治疗情况[例(%)] | 生命体征 | |||||||||||||||||||||||||||||
| 机械通气 | 深静脉置管 | 肾脏替代治疗 | 血管活性药物 使用>24 h | MAP(mmHg) | HR(次/min) | ||||||||||||||||||||||||||
| 死亡组 | 82(90.1) | 79(86.8) | 37(40.7) | 76(83.5) | 70(58, 77) | 127.8±25.5 | |||||||||||||||||||||||||
| 存活组 | 48(67.6) | 39(54.9) | 7(9.9) | 25(35.2) | 73(66, 80) | 116.2±25.0 | |||||||||||||||||||||||||
| t/Z/χ2值 | 12.664 | 20.367 | 19.006 | 39.397 | -2.415 | -2.892 | |||||||||||||||||||||||||
| P值 | 0.000 | 0.000 | 0.000 | 0.000 | 0.014 | 0.004 | |||||||||||||||||||||||||
| 组别 | 实验室资料 | ||||||||||||||||||||||||||||||
| P/F (mmHg) | WBC (×109/L) | NEUT% | Neut (×109/L) | Lymph (×109/L) | NLR | Lac (mmol/L) | |||||||||||||||||||||||||
| 死亡组 | 156(105, 208) | 14.6(10.2, 22.4) | 90.8(84.4, 94.2) | 12.5(8.7, 20.9) | 0.5(0.3, 0.8) | 17(10, 37) | 3.9(2.2, 9.2) | ||||||||||||||||||||||||
| 存活组 | 195(160, 270) | 17.5(11.7, 25.0) | 92.5(89.1, 95.2) | 16.3(10.5, 22.7) | 0.6(0.4, 0.8) | 26.5(15, 40) | 2.9(1.9, 4.9) | ||||||||||||||||||||||||
| t/Z/χ2值 | -3.717 | -2.079 | 1.943 | -1.944 | -0.756 | 1.896 | -2.306 | ||||||||||||||||||||||||
| P值 | 0.000 | 0.038 | 0.052 | 0.052 | 0.450 | 0.058 | 0.021 | ||||||||||||||||||||||||
| 组别 | 实验室资料 | ||||||||||||||||||||||||||||||
| PCT(μg/L) | PLT(×109/L) | D-Dimer(mg/L) | Alb(g/L) | TBil(μmol/L) | Cr(μmol/L) | ||||||||||||||||||||||||||
| 死亡组 | 19.7(4.6, 86.3) | 108(48, 176) | 8.3(4.7, 18.2) | 25.9±5.4 | 22.8(12.8, 41.5) | 156(94.2, 262.1) | |||||||||||||||||||||||||
| 存活组 | 17.3(2.8, 51) | 134(68, 204) | 6(2.9, 13.8) | 25.8±6.3 | 21.9(11, 37.7) | 91.4(62.7, 147.8) | |||||||||||||||||||||||||
| t/Z/χ2值 | -0.999 | -1.965 | -2.225 | -0.143 | -0.439 | -4.159 | |||||||||||||||||||||||||
| P值 | 0.318 | 0.049 | 0.026 | 0.889 | 0.661 | 0.000 | |||||||||||||||||||||||||
Tab. 2 Univariate analysis of the prognosis of sepsis patients with BSI
| 组别 | 例数 | 性别[例(%)] | 年龄 (岁) | 社区获得性 [例(%)] | 非ICU医院 获得性 [例(%)] | ICU获得性 [例(%)] | 评分(分) | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | SOFA 评分 | APACHEⅡ 评分 | mNUTRIC 评分 | SIC 评分 | ||||||||||||||||||||||||||
| 死亡组 | 91 | 55(60.4) | 36(39.6) | 71(63, 76) | 45(49.5) | 19(20.9) | 27(29.7) | 13(11, 15) | 25(20, 31) | 7(6, 8) | 4(3, 6) | ||||||||||||||||||||
| 存活组 | 71 | 37(52.1) | 34(47.9) | 63(50, 71) | 50(70.4) | 11(15.5) | 10(14.1) | 8(6, 11) | 18(14, 22) | 5(3, 6) | 4(3, 5) | ||||||||||||||||||||
| t/Z/χ2值 | 1.127 | -3.384 | 7.233 | 0.767 | 5.497 | -7.157 | -6.523 | -5.700 | -2.724 | ||||||||||||||||||||||
| P值 | 0.288 | 0.001 | 0.007 | 0.381 | 0.019 | 0.000 | 0.000 | 0.000 | 0.006 | ||||||||||||||||||||||
| 组别 | 治疗情况[例(%)] | 生命体征 | |||||||||||||||||||||||||||||
| 机械通气 | 深静脉置管 | 肾脏替代治疗 | 血管活性药物 使用>24 h | MAP(mmHg) | HR(次/min) | ||||||||||||||||||||||||||
| 死亡组 | 82(90.1) | 79(86.8) | 37(40.7) | 76(83.5) | 70(58, 77) | 127.8±25.5 | |||||||||||||||||||||||||
| 存活组 | 48(67.6) | 39(54.9) | 7(9.9) | 25(35.2) | 73(66, 80) | 116.2±25.0 | |||||||||||||||||||||||||
| t/Z/χ2值 | 12.664 | 20.367 | 19.006 | 39.397 | -2.415 | -2.892 | |||||||||||||||||||||||||
| P值 | 0.000 | 0.000 | 0.000 | 0.000 | 0.014 | 0.004 | |||||||||||||||||||||||||
| 组别 | 实验室资料 | ||||||||||||||||||||||||||||||
| P/F (mmHg) | WBC (×109/L) | NEUT% | Neut (×109/L) | Lymph (×109/L) | NLR | Lac (mmol/L) | |||||||||||||||||||||||||
| 死亡组 | 156(105, 208) | 14.6(10.2, 22.4) | 90.8(84.4, 94.2) | 12.5(8.7, 20.9) | 0.5(0.3, 0.8) | 17(10, 37) | 3.9(2.2, 9.2) | ||||||||||||||||||||||||
| 存活组 | 195(160, 270) | 17.5(11.7, 25.0) | 92.5(89.1, 95.2) | 16.3(10.5, 22.7) | 0.6(0.4, 0.8) | 26.5(15, 40) | 2.9(1.9, 4.9) | ||||||||||||||||||||||||
| t/Z/χ2值 | -3.717 | -2.079 | 1.943 | -1.944 | -0.756 | 1.896 | -2.306 | ||||||||||||||||||||||||
| P值 | 0.000 | 0.038 | 0.052 | 0.052 | 0.450 | 0.058 | 0.021 | ||||||||||||||||||||||||
| 组别 | 实验室资料 | ||||||||||||||||||||||||||||||
| PCT(μg/L) | PLT(×109/L) | D-Dimer(mg/L) | Alb(g/L) | TBil(μmol/L) | Cr(μmol/L) | ||||||||||||||||||||||||||
| 死亡组 | 19.7(4.6, 86.3) | 108(48, 176) | 8.3(4.7, 18.2) | 25.9±5.4 | 22.8(12.8, 41.5) | 156(94.2, 262.1) | |||||||||||||||||||||||||
| 存活组 | 17.3(2.8, 51) | 134(68, 204) | 6(2.9, 13.8) | 25.8±6.3 | 21.9(11, 37.7) | 91.4(62.7, 147.8) | |||||||||||||||||||||||||
| t/Z/χ2值 | -0.999 | -1.965 | -2.225 | -0.143 | -0.439 | -4.159 | |||||||||||||||||||||||||
| P值 | 0.318 | 0.049 | 0.026 | 0.889 | 0.661 | 0.000 | |||||||||||||||||||||||||
| 指标 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 年龄 | 0.067 | 0.025 | 7.442 | 0.006 | 1.070 | 1.019 | 1.123 |
| SOFA评分 | 0.263 | 0.133 | 3.889 | 0.049 | 1.301 | 1.002 | 1.689 |
| APACHEⅡ评分 | 0.164 | 0.082 | 3.973 | 0.046 | 1.179 | 1.003 | 1.385 |
| mNUTRIC评分 | 0.122 | 0.286 | 6.074 | 0.014 | 1.105 | 1.007 | 1.206 |
| P/F | -0.006 | 0.003 | 4.046 | 0.044 | 0.994 | 0.989 | 1.000 |
| WBC | -0.062 | 0.024 | 6.862 | 0.009 | 0.940 | 0.897 | 0.984 |
| 使用血管活性药物>24 h | 1.417 | 0.581 | 5.952 | 0.015 | 4.125 | 1.321 | 12.878 |
Tab.3 Multivariate logistic analysis of 28-day prognosis in sepsis patients with BSI
| 指标 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 年龄 | 0.067 | 0.025 | 7.442 | 0.006 | 1.070 | 1.019 | 1.123 |
| SOFA评分 | 0.263 | 0.133 | 3.889 | 0.049 | 1.301 | 1.002 | 1.689 |
| APACHEⅡ评分 | 0.164 | 0.082 | 3.973 | 0.046 | 1.179 | 1.003 | 1.385 |
| mNUTRIC评分 | 0.122 | 0.286 | 6.074 | 0.014 | 1.105 | 1.007 | 1.206 |
| P/F | -0.006 | 0.003 | 4.046 | 0.044 | 0.994 | 0.989 | 1.000 |
| WBC | -0.062 | 0.024 | 6.862 | 0.009 | 0.940 | 0.897 | 0.984 |
| 使用血管活性药物>24 h | 1.417 | 0.581 | 5.952 | 0.015 | 4.125 | 1.321 | 12.878 |
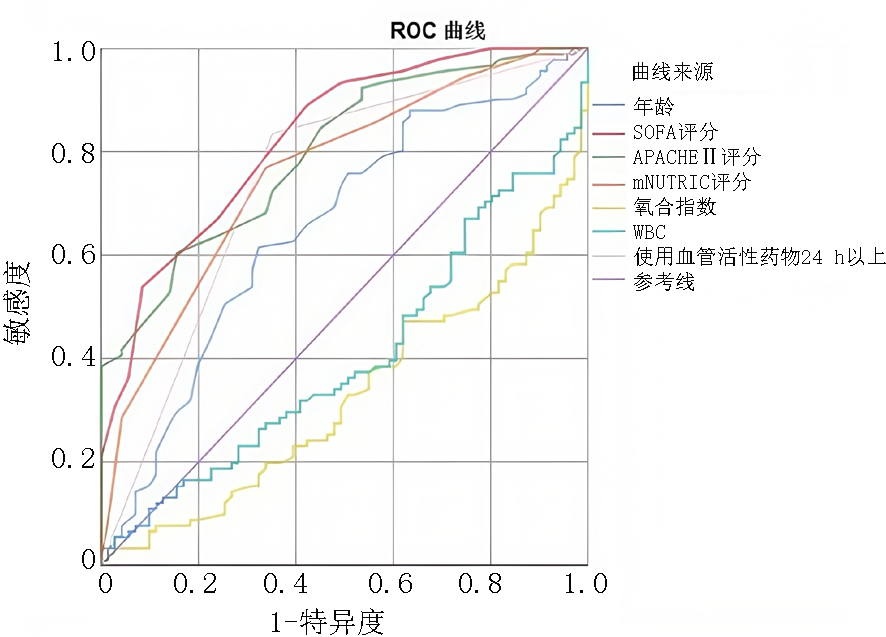
| 预测项目 | AUC | P值 | 95%CI | 敏感度 | 特异度 | 约登指数 | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 年龄 | 0.655 | 0.001 | 0.570 | 0.741 | 0.615 | 0.676 | 67.50 |
| SOFA评分 | 0.827 | 0.000 | 0.765 | 0.889 | 0.890 | 0.577 | 9.50 |
| APACHEⅡ评分 | 0.799 | 0.000 | 0.733 | 0.865 | 0.604 | 0.845 | 23.50 |
| mNUTRIC评分 | 0.758 | 0.000 | 0.684 | 0.832 | 0.769 | 0.662 | 5.50 |
| P/F | 0.330 | 0.000 | 0.248 | 0.412 | 0.582 | 0.127 | 133.50 |
| WBC | 0.405 | 0.038 | 0.318 | 0.492 | 0.396 | 0.394 | 16.03 |
| 使用血管活性药物>24 h | 0.742 | 0.000 | 0.662 | 0.821 | 0.835 | 0.648 | - |
Tab.4 Predictive value of independent influencing factors for 28-day prognosis in sepsis patients with BSI
| 预测项目 | AUC | P值 | 95%CI | 敏感度 | 特异度 | 约登指数 | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 年龄 | 0.655 | 0.001 | 0.570 | 0.741 | 0.615 | 0.676 | 67.50 |
| SOFA评分 | 0.827 | 0.000 | 0.765 | 0.889 | 0.890 | 0.577 | 9.50 |
| APACHEⅡ评分 | 0.799 | 0.000 | 0.733 | 0.865 | 0.604 | 0.845 | 23.50 |
| mNUTRIC评分 | 0.758 | 0.000 | 0.684 | 0.832 | 0.769 | 0.662 | 5.50 |
| P/F | 0.330 | 0.000 | 0.248 | 0.412 | 0.582 | 0.127 | 133.50 |
| WBC | 0.405 | 0.038 | 0.318 | 0.492 | 0.396 | 0.394 | 16.03 |
| 使用血管活性药物>24 h | 0.742 | 0.000 | 0.662 | 0.821 | 0.835 | 0.648 | - |
| [1] | Zahar JR, Timsit JF, Garrouste-Orgeas M, et al. Outcomes in severe sepsis and patients with septic shock: Pathogen species and infection sites are not associated with mortality[J]. Crit Care Med, 2011, 39(8):1886-1895. |
| [2] | 李雪, 赵涛, 吴嘉荔, 等. 早期降钙素、中性粒细胞百分比、血清乳酸对血流感染的脓毒症患者预后判断价值[J]. 糖尿病天地, 2019, 16(2):7-8. |
| [3] | 赵磊, 盛博, 李丽娟, 等. 血流感染脓毒症患者炎症因子水平与疾病严重程度相关性研究[J]. 中华医院感染学杂志, 2015, (17):3841-3844. |
| [4] | 钟敏林. 血流感染脓毒症患者的证治特点与预后相关性分析[D]. 广州: 广州中医药大学, 2022. |
| [5] | Vallés J, Ferrer R. Bloodstream infection in the ICU[J]. Infect Dis Clin North Am, 2009, 23(3):557-569. |
| [6] | Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021[J]. Crit Care Med, 2021, 49(11):e1063-e1143. |
| [7] |
Gouel-Cheron A, Swihart BJ, Warner S, et al. Epidemiology of ICU-onset bloodstream infection: Prevalence, pathogens, and risk factors among 150, 948 ICU patients at 85 U.S. hospitals[J]. Crit Care Med, 2022, 50(12):1725-1736.
doi: 10.1097/CCM.0000000000005662 pmid: 36190259 |
| [8] |
Yahav D, Eliakim-Raz N, Leibovici L, et al. Bloodstream infections in older patients[J]. Virulence, 2016, 7(3):341-352.
doi: 10.1080/21505594.2015.1132142 pmid: 26684392 |
| [9] | Moschou A, Ioannou P, Maraki S, et al. A prospective study of epidemiology characteristics and outcomes of bloodstream infections in older patients[J]. Australas J Ageing, 2021, 40(3):e182-e189. |
| [10] |
Cuesta JM, Singer M. The stress response and critical illness: A review[J]. Crit Care Med, 2012, 40(12):3283-3289.
doi: 10.1097/CCM.0b013e31826567eb pmid: 22975887 |
| [11] | Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine[J]. Intensive Care Med, 1996, 22(7):707-710. |
| [12] | Tauber SC, Djukic M, Gossner J, et al. Sepsis-associated encephalopathy and septic encephalitis: An update[J]. Expert Rev Anti Infect Ther, 2021, 19(2):215-231. |
| [13] | 王玲玲, 陈蕊, 董家辉, 等. mNUTRIC评分对老年脓毒症患者发生慢重症的预测价值测价值[J]. 中华急诊医学杂志, 2022, 31(1):73-77. |
| [14] |
Marchick MR, Kline JA, Jones AE. The significance of non-sustained hypotension in emergency department patients with sepsis[J]. Intensive Care Med, 2009, 35(7):1261-1264.
doi: 10.1007/s00134-009-1448-x pmid: 19238354 |
| [15] | 黄匀, 龚晨晨, 付建宇, 等. 重症监护病房血流感染预后危险因素分析[J]. 中华危重病急救医学, 2020, 32(12):1440-1444. |
| [16] | 吴丽丽, 梁群, 曹雪丹. 中医药保护脓毒症肺血管内皮细胞损伤的机制研究进展[J]. 中国中医急症, 2021, 30(1):172-175. |
| [17] | 陈瑞娟, 芮庆林, 郭涛, 等. 重症监护病房血流感染的临床特点和病原学分析[J]. 中国感染与化疗杂志, 2016, 16(6):673-679. |
| [18] | 希仁娜依·木哈塔尔, 丁巍, 邬超, 等. 重症感染后白细胞降低30例临床分析[J]. 新疆医学, 2019, 49(2):119-122. |
| [19] | 闫晶, 张珺, 张小彬, 等. 重症监护病房血流感染患者临床特点及预后影响因素分析[J]. 宁夏医学杂志, 2020, 42(4):322-325. |
| [20] |
Wagenlehner FM, Lichtenstern C, Rolfes C, et al. Diagnosis and management for urosepsis[J]. Int J Urol, 2013, 20(10):963-970.
doi: 10.1111/iju.12200 pmid: 23714209 |
| [21] | Buonacera A, Stancanelli B, Colaci M, et al. Neutrophil to lymphocyte ratio: An emerging marker of the relationships between the immune system and diseases[J]. Int J Mol Sci, 2022, 23(7):3636. |
| [22] |
Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives[J]. Bratisl Lek Listy, 2021, 122(7):474-488.
doi: 10.4149/BLL_2021_078 pmid: 34161115 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||