Clinical Focus ›› 2025, Vol. 40 ›› Issue (11): 999-1005.doi: 10.3969/j.issn.1004-583X.2025.11.005
Previous Articles Next Articles
Association between exogenous insulin autoimmune syndrome and diabetic kidney disease
Ruan Peng, Tayyaba Khan, Zhang Nenghan, Zhang Chunyan, Han Tuo, Wang Congxia( )
)
- Department of Cardiovascular Medicine, the Second Affiliated Hospital of Xi'an Jiaotong University, Xi'an 710016,China
-
Received:2025-09-12Online:2025-11-20Published:2025-12-02 -
Contact:Wang Congxia E-mail:wcx622@163.com
CLC Number:
Cite this article
Ruan Peng, Tayyaba Khan, Zhang Nenghan, Zhang Chunyan, Han Tuo, Wang Congxia. Association between exogenous insulin autoimmune syndrome and diabetic kidney disease[J]. Clinical Focus, 2025, 40(11): 999-1005.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.lchc.cn/EN/10.3969/j.issn.1004-583X.2025.11.005
| 变量 | 总体( | 对照组( | EIAS组( | ||
|---|---|---|---|---|---|
| 年龄(岁) | 51.3±17.6 | 47.1±16.3 | 60.8±17.0 | 17.004 | <0.01 |
| 性别[例(%)] | |||||
| 男性 女性 | 66(57.4) 49(42.6) | 49(62.0) 30(38.0) | 17(47.2) 19(52.8) | 2.216 | 0.137 |
| BMI(kg/m2) | 22.9±3.3 | 22.6±3.2 | 23.5±3.5 | 2.133 | 0.147 |
| 糖尿病类型[例(%)] | |||||
| T1DM | 11(9.6) | 8(10.1) | 3(8.3) | ||
| T2DM | 92(80.0) | 60(75.9) | 32(88.9) | 0.157 | |
| LADA | 12(10.4) | 11(13.9) | 1(2.8) | ||
| 病程(年) | 10.0(2.0, 16.0) | 6.0(1.0, 14.0) | 12.5(7.8, 20.0) | 7.876 | 0.005 |
| 胰岛素剂量(IU) | 27.0(10.0, 42.0) | 20.0(0.0, 38.0) | 36.5(25.5, 49.2) | 11.414 | <0.01 |
| 吸烟史[例(%)] | 43(37.4) | 33(41.8) | 10(27.8) | 2.069 | 0.150 |
| 饮酒史[例(%)] | 20(17.4) | 17(21.5) | 3(8.3) | 2.993 | 0.084 |
| 血小板计数(×109/L) | 222.6±63.6 | 222.8±63.5 | 222.2±64.6 | 0.002 | 0.962 |
| 中性粒细胞计数(×109/L) | 4.0±1.5 | 3.9±1.6 | 4.3±1.3 | 1.216 | 0.272 |
| 单核细胞计数(×109/L) | 0.4±0.1 | 0.4±0.1 | 0.4±0.1 | 0.001 | 0.971 |
| 淋巴细胞计数(×109/L) | 1.7±0.7 | 1.7±0.7 | 1.6±0.7 | 0.451 | 0.503 |
| 谷丙转氨酶(IU/L) | 18.5(13.2, 27.8) | 17.0(13.0, 27.5) | 20.0(15.0, 27.5) | 0.474 | 0.491 |
| 谷草转氨酶(IU/L) | 21.9±12.3 | 21.8±13.8 | 22.1±8.2 | 0.022 | 0.883 |
| 白蛋白(g/L) | 44.6±3.7 | 44.7±3.3 | 44.2±4.5 | 0.486 | 0.487 |
| 血尿酸(μmol/L) | 293.5±101.3 | 287.9±110.0 | 305.6±79.1 | 0.687 | 0.409 |
| 尿素氮(mmol/L) | 5.5±2.1 | 5.5±2.1 | 5.6±2.1 | 0.107 | 0.744 |
| 血肌酐(mmol/L) | 66.0±27.6 | 63.1±28.7 | 72.6±23.9 | 2.951 | 0.089 |
| 肾小球滤过率[ml/(min·1.73 m2)] | 99.6±25.5 | 105.0±25.1 | 87.4±22.2 | 11.983 | <0.01 |
| 总胆固醇(mmol/L) | 4.6±1.6 | 4.8±1.7 | 4.3±1.3 | 1.960 | 0.164 |
| 甘油三酯(mmol/L) | 1.4(1.0, 2.1) | 1.4(1.0, 2.4) | 1.4(0.9, 1.7) | 0.946 | 0.331 |
| 低密度脂蛋白胆固醇(mmol/L) | 1.3±0.3 | 1.3±0.3 | 1.3±0.3 | 0.029 | 0.865 |
| 高密度脂蛋白胆固醇(mmol/L) | 2.7±1.0 | 2.8±1.0 | 2.5±1.0 | 1.275 | 0.261 |
| 空腹血糖(mmol/L) | 11.5±5.3 | 12.4±5.9 | 9.6±3.0 | 7.616 | 0.007 |
| 空腹胰岛素(mU/L) | 4.3(2.1, 14.7) | 2.9(1.3, 6.2) | 13.1(5.4, 35.0) | 22.303 | <0.01 |
| 空腹C肽(ng/ml) | 0.9(0.6, 1.6) | 0.8(0.6, 1.5) | 1.1(0.7, 1.8) | 3.463 | 0.063 |
| 餐后2 h血糖(mmol/L) | 15.1±4.5 | 15.0±4.2 | 15.4±5.2 | 0.109 | 0.742 |
| 餐后2 h胰岛(mU/L) | 10.5(4.5, 20.4) | 8.2(3.6, 14.7) | 19.5(10.8, 41.8) | 14.863 | <0.01 |
| 餐后2 h C肽(ng/ml) | 1.8(1.2, 3.0) | 1.8(0.9, 2.9) | 2.1(1.5, 3.5) | 2.546 | 0.111 |
| 糖化血红蛋白(%) | 9.4±2.3 | 9.9±2.5 | 8.3±1.6 | 13.022 | <0.01 |
| HOMA-IR | 2.3(0.9, 6.1) | 1.8(0.7, 3.6) | 6.1(2.3, 14.2) | 17.133 | <0.01 |
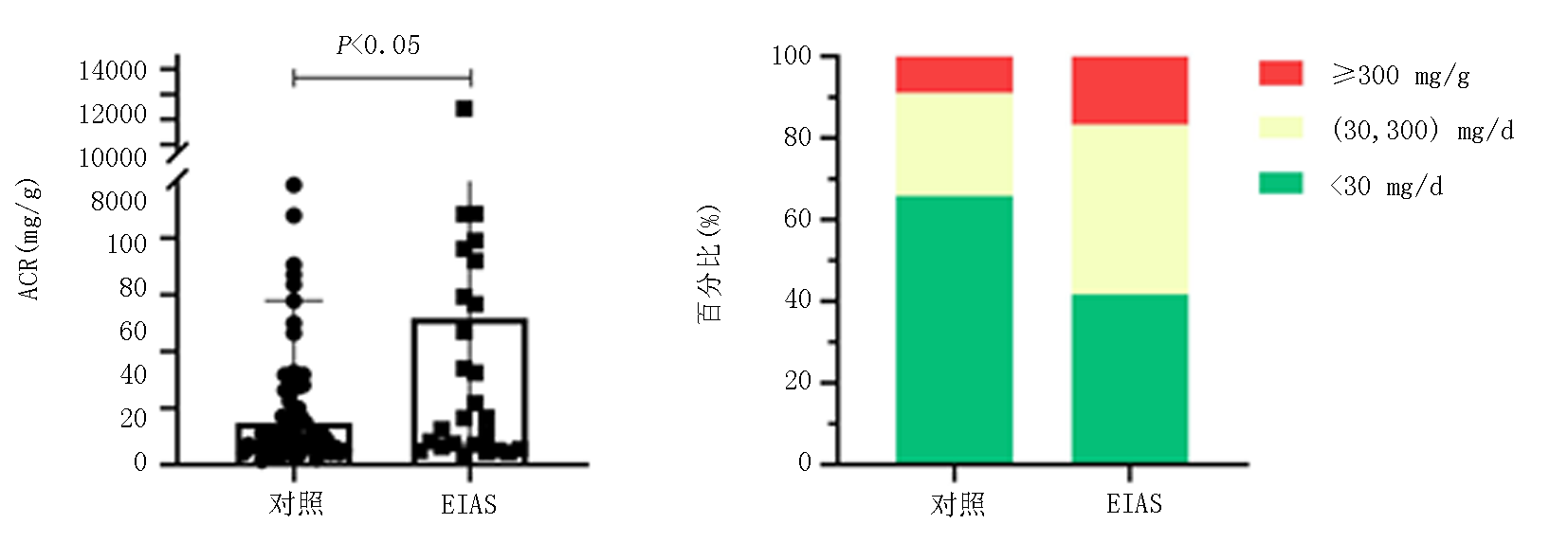
| ACR(mg/g) | 17.1(7.1, 83.5) | 14.8(6.6, 53.9) | 51.8(8.1, 114.6) | 4.034 | 0.045 |
| ACR分级[例(%)] | |||||
| <30 mg/g | 67(58.3) | 52(65.8) | 15(41.7) | ||
| [30, 300) mg/g | 35(30.4) | 20(25.3) | 15(41.7) | 0.051 | |
| ≥300 mg/g | 13(11.3) | 7(8.9) | 6(16.7) |
Tab.1 Comparison of clinical characteristics between the EIAS group and the control group
| 变量 | 总体( | 对照组( | EIAS组( | ||
|---|---|---|---|---|---|
| 年龄(岁) | 51.3±17.6 | 47.1±16.3 | 60.8±17.0 | 17.004 | <0.01 |
| 性别[例(%)] | |||||
| 男性 女性 | 66(57.4) 49(42.6) | 49(62.0) 30(38.0) | 17(47.2) 19(52.8) | 2.216 | 0.137 |
| BMI(kg/m2) | 22.9±3.3 | 22.6±3.2 | 23.5±3.5 | 2.133 | 0.147 |
| 糖尿病类型[例(%)] | |||||
| T1DM | 11(9.6) | 8(10.1) | 3(8.3) | ||
| T2DM | 92(80.0) | 60(75.9) | 32(88.9) | 0.157 | |
| LADA | 12(10.4) | 11(13.9) | 1(2.8) | ||
| 病程(年) | 10.0(2.0, 16.0) | 6.0(1.0, 14.0) | 12.5(7.8, 20.0) | 7.876 | 0.005 |
| 胰岛素剂量(IU) | 27.0(10.0, 42.0) | 20.0(0.0, 38.0) | 36.5(25.5, 49.2) | 11.414 | <0.01 |
| 吸烟史[例(%)] | 43(37.4) | 33(41.8) | 10(27.8) | 2.069 | 0.150 |
| 饮酒史[例(%)] | 20(17.4) | 17(21.5) | 3(8.3) | 2.993 | 0.084 |
| 血小板计数(×109/L) | 222.6±63.6 | 222.8±63.5 | 222.2±64.6 | 0.002 | 0.962 |
| 中性粒细胞计数(×109/L) | 4.0±1.5 | 3.9±1.6 | 4.3±1.3 | 1.216 | 0.272 |
| 单核细胞计数(×109/L) | 0.4±0.1 | 0.4±0.1 | 0.4±0.1 | 0.001 | 0.971 |
| 淋巴细胞计数(×109/L) | 1.7±0.7 | 1.7±0.7 | 1.6±0.7 | 0.451 | 0.503 |
| 谷丙转氨酶(IU/L) | 18.5(13.2, 27.8) | 17.0(13.0, 27.5) | 20.0(15.0, 27.5) | 0.474 | 0.491 |
| 谷草转氨酶(IU/L) | 21.9±12.3 | 21.8±13.8 | 22.1±8.2 | 0.022 | 0.883 |
| 白蛋白(g/L) | 44.6±3.7 | 44.7±3.3 | 44.2±4.5 | 0.486 | 0.487 |
| 血尿酸(μmol/L) | 293.5±101.3 | 287.9±110.0 | 305.6±79.1 | 0.687 | 0.409 |
| 尿素氮(mmol/L) | 5.5±2.1 | 5.5±2.1 | 5.6±2.1 | 0.107 | 0.744 |
| 血肌酐(mmol/L) | 66.0±27.6 | 63.1±28.7 | 72.6±23.9 | 2.951 | 0.089 |
| 肾小球滤过率[ml/(min·1.73 m2)] | 99.6±25.5 | 105.0±25.1 | 87.4±22.2 | 11.983 | <0.01 |
| 总胆固醇(mmol/L) | 4.6±1.6 | 4.8±1.7 | 4.3±1.3 | 1.960 | 0.164 |
| 甘油三酯(mmol/L) | 1.4(1.0, 2.1) | 1.4(1.0, 2.4) | 1.4(0.9, 1.7) | 0.946 | 0.331 |
| 低密度脂蛋白胆固醇(mmol/L) | 1.3±0.3 | 1.3±0.3 | 1.3±0.3 | 0.029 | 0.865 |
| 高密度脂蛋白胆固醇(mmol/L) | 2.7±1.0 | 2.8±1.0 | 2.5±1.0 | 1.275 | 0.261 |
| 空腹血糖(mmol/L) | 11.5±5.3 | 12.4±5.9 | 9.6±3.0 | 7.616 | 0.007 |
| 空腹胰岛素(mU/L) | 4.3(2.1, 14.7) | 2.9(1.3, 6.2) | 13.1(5.4, 35.0) | 22.303 | <0.01 |
| 空腹C肽(ng/ml) | 0.9(0.6, 1.6) | 0.8(0.6, 1.5) | 1.1(0.7, 1.8) | 3.463 | 0.063 |
| 餐后2 h血糖(mmol/L) | 15.1±4.5 | 15.0±4.2 | 15.4±5.2 | 0.109 | 0.742 |
| 餐后2 h胰岛(mU/L) | 10.5(4.5, 20.4) | 8.2(3.6, 14.7) | 19.5(10.8, 41.8) | 14.863 | <0.01 |
| 餐后2 h C肽(ng/ml) | 1.8(1.2, 3.0) | 1.8(0.9, 2.9) | 2.1(1.5, 3.5) | 2.546 | 0.111 |
| 糖化血红蛋白(%) | 9.4±2.3 | 9.9±2.5 | 8.3±1.6 | 13.022 | <0.01 |
| HOMA-IR | 2.3(0.9, 6.1) | 1.8(0.7, 3.6) | 6.1(2.3, 14.2) | 17.133 | <0.01 |
| ACR(mg/g) | 17.1(7.1, 83.5) | 14.8(6.6, 53.9) | 51.8(8.1, 114.6) | 4.034 | 0.045 |
| ACR分级[例(%)] | |||||
| <30 mg/g | 67(58.3) | 52(65.8) | 15(41.7) | ||
| [30, 300) mg/g | 35(30.4) | 20(25.3) | 15(41.7) | 0.051 | |
| ≥300 mg/g | 13(11.3) | 7(8.9) | 6(16.7) |
| 降糖药物 | 总体( | 对照组( | EIAS组( | χ2值 | |
|---|---|---|---|---|---|
| 门冬胰岛素 | 57(49.6) | 34(43) | 23(63.9) | 4.301 | 0.038 |
| 甘精胰岛素 | 46(40.0) | 28(35.4) | 18(50.0) | 2.184 | 0.139 |
| 赖脯胰岛素 | 8(7.0) | 6(7.6) | 2(5.6) | - | 0.999 |
| 地特胰岛素 | 13(11.3) | 7(8.9) | 6(16.7) | - | 0.223 |
| 德古胰岛素 | 40(34.8) | 31(39.2) | 9(25.0) | 2.211 | 0.137 |
| 预混人胰岛素 | 19(16.5) | 9(11.4) | 10(27.8) | 4.814 | 0.028 |
| 二甲双胍 | 59(51.3) | 43(54.4) | 16(44.4) | 0.987 | 0.320 |
| α糖苷酶抑制剂 | 31(27.0) | 21(26.6) | 10(27.8) | 0.018 | 0.893 |
| 钠-葡萄糖共转运蛋白2抑制剂 | 16(13.9) | 10(12.7) | 6(16.7) | 0.332 | 0.565 |
| 二肽基肽酶4抑制剂 | 13(11.3) | 9(11.4) | 4(11.1) | - | 1.000 |
| 磺脲类 | 5(4.3) | 3(3.8) | 2(5.6) | - | 0.648 |
| 噻唑烷二酮类 | 5(4.3) | 5(6.3) | 0(0.0) | - | 0.323 |
| 胰高血糖素样肽1受体激动剂 | 8(7.0) | 5(6.3) | 3(8.3) | - | 0.704 |
Tab.2 Use of hypoglycemic drugs in the EIAS and control groups(n, %)
| 降糖药物 | 总体( | 对照组( | EIAS组( | χ2值 | |
|---|---|---|---|---|---|
| 门冬胰岛素 | 57(49.6) | 34(43) | 23(63.9) | 4.301 | 0.038 |
| 甘精胰岛素 | 46(40.0) | 28(35.4) | 18(50.0) | 2.184 | 0.139 |
| 赖脯胰岛素 | 8(7.0) | 6(7.6) | 2(5.6) | - | 0.999 |
| 地特胰岛素 | 13(11.3) | 7(8.9) | 6(16.7) | - | 0.223 |
| 德古胰岛素 | 40(34.8) | 31(39.2) | 9(25.0) | 2.211 | 0.137 |
| 预混人胰岛素 | 19(16.5) | 9(11.4) | 10(27.8) | 4.814 | 0.028 |
| 二甲双胍 | 59(51.3) | 43(54.4) | 16(44.4) | 0.987 | 0.320 |
| α糖苷酶抑制剂 | 31(27.0) | 21(26.6) | 10(27.8) | 0.018 | 0.893 |
| 钠-葡萄糖共转运蛋白2抑制剂 | 16(13.9) | 10(12.7) | 6(16.7) | 0.332 | 0.565 |
| 二肽基肽酶4抑制剂 | 13(11.3) | 9(11.4) | 4(11.1) | - | 1.000 |
| 磺脲类 | 5(4.3) | 3(3.8) | 2(5.6) | - | 0.648 |
| 噻唑烷二酮类 | 5(4.3) | 5(6.3) | 0(0.0) | - | 0.323 |
| 胰高血糖素样肽1受体激动剂 | 8(7.0) | 5(6.3) | 3(8.3) | - | 0.704 |
| 变量 | 总体( | ACR<30 mg/g( | ACR≥30 mg/g( | ||
|---|---|---|---|---|---|
| 年龄(岁) | 51.3±17.6 | 46.6±16.2 | 57.9±17.6 | 12.530 | <0.01 |
| 性别[例(%)] | |||||
| 男性 女性 | 66(57.4) 49(42.6) | 37(55.2) 30(44.8) | 29(60.4) 19(39.6) | 0.308 | 0.579 |
| BMI(kg/m2) | 22.9±3.3 | 22.7±3.0 | 23.2±3.7 | 0.579 | 0.448 |
| 糖尿病类型[例(%)] | |||||
| T1DM | 11(9.6) | 7(10.4) | 4(8.3) | ||
| T2DM | 92(80.0) | 52(77.6) | 40(83.3) | 0.785 | |
| LADA | 12(10.4) | 8(11.9) | 4(8.3) | ||
| 病程(年) | 10.0(2.0, 16.0) | 7.0(1.0, 12.5) | 10.5(5.0, 20.0) | 7.025 | 0.008 |
| 胰岛素剂量(IU) | 27.0(10.0, 42.0) | 26.0(0.0, 40.5) | 30.0(14.8, 46.2) | 1.543 | 0.214 |
| 吸烟史[例(%)] | 43(37.4) | 23(34.3) | 20(41.7) | 0.643 | 0.423 |
| 饮酒史[例(%)] | 20(17.4) | 12(17.9) | 8(16.7) | 0.030 | 0.862 |
| 血小板计数(×109/L) | 222.6±63.6 | 224.3±68.2 | 220.1±57.0 | 0.122 | 0.728 |
| 中性粒细胞计数(×109/L) | 4.0±1.5 | 3.9±1.6 | 4.2±1.3 | 1.234 | 0.269 |
| 单核细胞计数(×109/L) | 0.4±0.1 | 0.4±0.1 | 0.4±0.1 | 3.659 | 0.058 |
| 淋巴细胞计数(×109/L) | 1.7±0.7 | 1.7±0.6 | 1.8±0.8 | 0.834 | 0.363 |
| 谷丙转氨酶(IU/L) | 18.5(13.2, 27.8) | 19.0(13.0, 26.5) | 17.0(14.0, 28.0) | 0.010 | 1.000 |
| 谷草转氨酶(IU/L) | 21.9±12.3 | 20.2±7.7 | 24.3±16.7 | 3.055 | 0.083 |
| 白蛋白(g/L) | 44.6±3.7 | 45.1±3.1 | 43.9±4.3 | 2.982 | 0.087 |
| 血尿酸(μmol/L) | 293.5±101.3 | 280.7±96.4 | 311.2±106.3 | 2.337 | 0.129 |
| 尿素氮(mmol/L) | 5.5±2.1 | 5.0±1.6 | 6.2±2.5 | 9.870 | 0.002 |
| 血肌酐(mmol/L) | 66.0±27.6 | 60.9±17.0 | 73.3±36.9 | 5.847 | 0.017 |
| 肾小球滤过率[ml/(min·1.73 m2)] | 99.6±25.5 | 105.4±23.0 | 91.6±26.9 | 8.073 | 0.005 |
| 总胆固醇(mmol/L) | 4.6±1.6 | 4.3±1.1 | 5.0±2.0 | 5.989 | 0.016 |
| 甘油三酯(mmol/L) | 1.4(1.0, 2.1) | 1.4(0.9, 1.9) | 1.5(1.1, 2.5) | 1.196 | 0.274 |
| 低密度脂蛋白胆固醇(mmol/L) | 1.3±0.3 | 1.2±0.3 | 1.3±0.3 | 0.511 | 0.476 |
| 高密度脂蛋白胆固醇(mmol/L) | 2.7±1.0 | 2.6±0.9 | 2.9±1.1 | 2.612 | 0.109 |
| 空腹血糖(mmol/L) | 11.5±5.3 | 11.6±5.5 | 11.5±5.2 | 0.006 | 0.938 |
| 空腹胰岛素(mU/L) | 4.3(2.1, 14.7) | 3.2(2.0, 8.4) | 5.6(2.6, 31.9) | 4.781 | 0.029 |
| 空腹C肽(ng/ml) | 0.9(0.6, 1.6) | 0.8(0.6, 1.5) | 1.0(0.6, 1.7) | 0.235 | 0.628 |
| 餐后2 h血糖(mmol/L) | 15.1±4.5 | 15.6±5.1 | 14.4±3.3 | 1.731 | 0.191 |
| 餐后2 h胰岛(mU/L) | 10.5(4.5, 20.4) | 11.1(6.0, 20.1) | 8.7(2.8, 21.2) | 0.258 | 0.612 |
| 餐后2 h C肽(ng/ml) | 1.8(1.2, 3.0) | 2.0(1.3, 3.0) | 1.6(1.0, 3.2) | 0.932 | 0.334 |
| 糖化血红蛋白(%) | 9.4±2.3 | 9.2±2.2 | 9.7±2.5 | 1.125 | 0.291 |
| HOMA-IR | 2.3(0.9, 6.1) | 1.9(0.8, 4.2) | 3.3(1.0, 12.6) | 4.632 | 0.031 |
| ACR(mg/g) | 17.1(7.1, 83.5) | 7.7(5.1, 13.1) | 100.5(58.9, 444.1) | 83.173 | <0.01 |
| EIAS[例(%)] | 36(31.3) | 15(22.4) | 21(43.8) | 5.934 | 0.015 |
Tab.3 Comparison of clinical characteristics between different ACR subgroups
| 变量 | 总体( | ACR<30 mg/g( | ACR≥30 mg/g( | ||
|---|---|---|---|---|---|
| 年龄(岁) | 51.3±17.6 | 46.6±16.2 | 57.9±17.6 | 12.530 | <0.01 |
| 性别[例(%)] | |||||
| 男性 女性 | 66(57.4) 49(42.6) | 37(55.2) 30(44.8) | 29(60.4) 19(39.6) | 0.308 | 0.579 |
| BMI(kg/m2) | 22.9±3.3 | 22.7±3.0 | 23.2±3.7 | 0.579 | 0.448 |
| 糖尿病类型[例(%)] | |||||
| T1DM | 11(9.6) | 7(10.4) | 4(8.3) | ||
| T2DM | 92(80.0) | 52(77.6) | 40(83.3) | 0.785 | |
| LADA | 12(10.4) | 8(11.9) | 4(8.3) | ||
| 病程(年) | 10.0(2.0, 16.0) | 7.0(1.0, 12.5) | 10.5(5.0, 20.0) | 7.025 | 0.008 |
| 胰岛素剂量(IU) | 27.0(10.0, 42.0) | 26.0(0.0, 40.5) | 30.0(14.8, 46.2) | 1.543 | 0.214 |
| 吸烟史[例(%)] | 43(37.4) | 23(34.3) | 20(41.7) | 0.643 | 0.423 |
| 饮酒史[例(%)] | 20(17.4) | 12(17.9) | 8(16.7) | 0.030 | 0.862 |
| 血小板计数(×109/L) | 222.6±63.6 | 224.3±68.2 | 220.1±57.0 | 0.122 | 0.728 |
| 中性粒细胞计数(×109/L) | 4.0±1.5 | 3.9±1.6 | 4.2±1.3 | 1.234 | 0.269 |
| 单核细胞计数(×109/L) | 0.4±0.1 | 0.4±0.1 | 0.4±0.1 | 3.659 | 0.058 |
| 淋巴细胞计数(×109/L) | 1.7±0.7 | 1.7±0.6 | 1.8±0.8 | 0.834 | 0.363 |
| 谷丙转氨酶(IU/L) | 18.5(13.2, 27.8) | 19.0(13.0, 26.5) | 17.0(14.0, 28.0) | 0.010 | 1.000 |
| 谷草转氨酶(IU/L) | 21.9±12.3 | 20.2±7.7 | 24.3±16.7 | 3.055 | 0.083 |
| 白蛋白(g/L) | 44.6±3.7 | 45.1±3.1 | 43.9±4.3 | 2.982 | 0.087 |
| 血尿酸(μmol/L) | 293.5±101.3 | 280.7±96.4 | 311.2±106.3 | 2.337 | 0.129 |
| 尿素氮(mmol/L) | 5.5±2.1 | 5.0±1.6 | 6.2±2.5 | 9.870 | 0.002 |
| 血肌酐(mmol/L) | 66.0±27.6 | 60.9±17.0 | 73.3±36.9 | 5.847 | 0.017 |
| 肾小球滤过率[ml/(min·1.73 m2)] | 99.6±25.5 | 105.4±23.0 | 91.6±26.9 | 8.073 | 0.005 |
| 总胆固醇(mmol/L) | 4.6±1.6 | 4.3±1.1 | 5.0±2.0 | 5.989 | 0.016 |
| 甘油三酯(mmol/L) | 1.4(1.0, 2.1) | 1.4(0.9, 1.9) | 1.5(1.1, 2.5) | 1.196 | 0.274 |
| 低密度脂蛋白胆固醇(mmol/L) | 1.3±0.3 | 1.2±0.3 | 1.3±0.3 | 0.511 | 0.476 |
| 高密度脂蛋白胆固醇(mmol/L) | 2.7±1.0 | 2.6±0.9 | 2.9±1.1 | 2.612 | 0.109 |
| 空腹血糖(mmol/L) | 11.5±5.3 | 11.6±5.5 | 11.5±5.2 | 0.006 | 0.938 |
| 空腹胰岛素(mU/L) | 4.3(2.1, 14.7) | 3.2(2.0, 8.4) | 5.6(2.6, 31.9) | 4.781 | 0.029 |
| 空腹C肽(ng/ml) | 0.9(0.6, 1.6) | 0.8(0.6, 1.5) | 1.0(0.6, 1.7) | 0.235 | 0.628 |
| 餐后2 h血糖(mmol/L) | 15.1±4.5 | 15.6±5.1 | 14.4±3.3 | 1.731 | 0.191 |
| 餐后2 h胰岛(mU/L) | 10.5(4.5, 20.4) | 11.1(6.0, 20.1) | 8.7(2.8, 21.2) | 0.258 | 0.612 |
| 餐后2 h C肽(ng/ml) | 1.8(1.2, 3.0) | 2.0(1.3, 3.0) | 1.6(1.0, 3.2) | 0.932 | 0.334 |
| 糖化血红蛋白(%) | 9.4±2.3 | 9.2±2.2 | 9.7±2.5 | 1.125 | 0.291 |
| HOMA-IR | 2.3(0.9, 6.1) | 1.9(0.8, 4.2) | 3.3(1.0, 12.6) | 4.632 | 0.031 |
| ACR(mg/g) | 17.1(7.1, 83.5) | 7.7(5.1, 13.1) | 100.5(58.9, 444.1) | 83.173 | <0.01 |
| EIAS[例(%)] | 36(31.3) | 15(22.4) | 21(43.8) | 5.934 | 0.015 |
| 变量 | 单因素回归 | 多因素回归 | |||
|---|---|---|---|---|---|
| 年龄 | 1.04(1.02~1.07) | 0.001 | 1.04(0.99~1.09) | 0.100 | |
| DM病程 | 1.07(1.02~1.12) | 0.005 | 1.06(0.98~1.15) | 0.171 | |
| 胰岛素剂量 | 1.01(0.99~1.03) | 0.253 | 1.00(0.98~1.02) | 0.968 | |
| 肾小球滤过率 | 0.98(0.96~0.99) | 0.008 | 0.98(0.96~1.01) | 0.179 | |
| 空腹血糖 | 1.00(0.93~1.07) | 0.937 | 1.04(0.92~1.16) | 0.549 | |
| 空腹胰岛素 | 1.01(1.00~1.03) | 0.095 | 1.00(0.99~1.01) | 0.923 | |
| 糖化血红蛋白 | 1.09(0.93~1.28) | 0.289 | 1.46(1.10~1.93) | 0.008 | |
| EIAS | 2.70(1.20~6.06) | 0.016 | 2.89(0.95~8.79) | 0.062 | |
Tab.4 Univariate and multivariate logistic regression of ACR elevation
| 变量 | 单因素回归 | 多因素回归 | |||
|---|---|---|---|---|---|
| 年龄 | 1.04(1.02~1.07) | 0.001 | 1.04(0.99~1.09) | 0.100 | |
| DM病程 | 1.07(1.02~1.12) | 0.005 | 1.06(0.98~1.15) | 0.171 | |
| 胰岛素剂量 | 1.01(0.99~1.03) | 0.253 | 1.00(0.98~1.02) | 0.968 | |
| 肾小球滤过率 | 0.98(0.96~0.99) | 0.008 | 0.98(0.96~1.01) | 0.179 | |
| 空腹血糖 | 1.00(0.93~1.07) | 0.937 | 1.04(0.92~1.16) | 0.549 | |
| 空腹胰岛素 | 1.01(1.00~1.03) | 0.095 | 1.00(0.99~1.01) | 0.923 | |
| 糖化血红蛋白 | 1.09(0.93~1.28) | 0.289 | 1.46(1.10~1.93) | 0.008 | |
| EIAS | 2.70(1.20~6.06) | 0.016 | 2.89(0.95~8.79) | 0.062 | |
| [1] | Cappellani D, Macchia E, Falorni A, et al. Insulin autoimmune syndrome(hirata disease): A comprehensive review fifty years after its first description[J]. Diabetes Metab Syndr Obes, 2020, 13:963-978. doi:10.2147/dmso.S219438. |
| [2] |
陈敏, 庄晓明, 窦京涛, 等. 胰岛素自身免疫综合征的临床特征比较分析[J]. 首都医科大学学报, 2012, 33(3):409-413.
doi: 10.3969/j.issn.1006-7795.2012.03.026 |
| [3] |
Uchigata Y, Omori Y, Nieda M, et al. HLA-DR4 genotype and insulin-processing in insulin autoimmune syndrome[J]. Lancet, 1992, 340(8833):1467. doi:10.1016/0140-6736(92)92654-x.
pmid: 1360579 |
| [4] | Jain N, Savani M, Agarwal M, et al. Methimazole-induced insulin autoimmune syndrome[J]. Ther Adv Endocrinol Metab, 2016, 7(4):178-181. doi:10.1177/2042018816658396. |
| [5] | 刘莉, 张木勋, 邵诗颖. 胰岛素自身免疫综合征1例诊治报告及文献复习[J]. 华中科技大学学报(医学版), 2018, 47(3):361-364. |
| [6] |
Shen Y, Song X, Ren Y. Insulin autoimmune syndrome induced by exogenous insulin injection: A four-case series[J]. BMC Endocr Disord, 2019, 19(1):148. doi:10.1186/s12902-019-0482-0.
pmid: 31883520 |
| [7] | 史晓伟, 王晓霞, 张定华, 等. 外源性胰岛素自身免疫综合征患者临床特征五例报道[J]. 中国糖尿病杂志, 2021, 29(11):850-854. |
| [8] |
Li Z, Yi D, Zheng L, et al. Analysis of the clinical characteristics of insulin autoimmune syndrome induced by exogenous insulin in diabetic patients[J]. Diabetol Metab Syndr, 2021, 13(1):38. doi:10.1186/s13098-021-00658-z.
pmid: 33827670 |
| [9] | Committee ADAPP. 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2022[J]. Diabetes Care, 2022, 45(Suppl 1):S17-s38. doi:10.2337/dc22-S002. |
| [10] |
Buzzetti R, Tuomi T, Mauricio D, et al. Management of latent autoimmune diabetes in adults: A consensus statement from an international expert panel[J]. Diabetes, 2020, 69(10):2037-2047. doi:10.2337/dbi20-0017.
pmid: 32847960 |
| [11] | Tahapary DL, Pratisthita LB, Fitri NA, et al. Challenges in the diagnosis of insulin resistance: Focusing on the role of HOMA-IR and tryglyceride/glucose index[J]. Diabetes Metab Syndr, 2022, 16(8):102581. doi:10.1016/j.dsx.2022.102581. |
| [12] | Wu HY, Peng YS, Chiang CK, et al. Diagnostic performance of random urine samples using albumin concentration vs ratio of albumin to creatinine for microalbuminuria screening in patients with diabetes mellitus: A systematic review and meta-analysis[J]. JAMA Intern Med, 2014, 174(7):1108-1115. doi:10.1001/jamainternmed.2014.1363. |
| [13] |
Censi S, Mian C, Betterle C. Insulin autoimmune syndrome: From diagnosis to clinical management[J]. Ann Transl Med, 2018, 6(17):335. doi:10.21037/atm.2018.07.32.
pmid: 30306074 |
| [14] | Liu Y, Ping F, Yu J, et al. Hypoglycemia caused by exogenous insulin antibody syndrome: A large single-center case series from China[J]. J Clin Endocrinol Metab, 2023, 108(3):713-717. doi:10.1210/clinem/dgac578. |
| [15] | 杨彩彩, 谷伟军, 吕朝晖, 等. 19例胰岛素自身免疫综合征的临床特点分析并文献复习[J]. 解放军医学院学报, 2020, 41(6):583-587. |
| [16] | Yamada Y, Kitayama K, Oyachi M, et al. Nationwide survey of endogenous hyperinsulinemic hypoglycemia in Japan(2017-2018): Congenital hyperinsulinism, insulinoma, non-insulinoma pancreatogenous hypoglycemia syndrome and insulin autoimmune syndrome(Hirata's disease)[J]. J Diabetes Investig, 2020, 11(3):554-563. doi:10.1111/jdi.13180. |
| [17] | Woo CY, Jeong JY, Jang JE, et al. Clinical features and causes of endogenous hyperinsulinemic hypoglycemia in Korea[J]. Diabetes Metab J, 2015, 39(2):126-131. doi:10.4093/dmj.2015.39.2.126. |
| [18] | 伊丽努尔·阿德尔江, 高静. 糖尿病患者胰岛素/C肽比值与胰岛素抗体的相关性研究[J]. 新疆医学, 2023, 53(8):907-911. |
| [19] |
Yuan T, Li J, Li M, et al. Insulin autoimmune syndrome diagnosis and therapy in a single chinese center[J]. Clin Ther, 2019, 41(5):920-928. doi:10.1016/j.clinthera.2019.03.009.
pmid: 30992145 |
| [20] |
Marzinotto I, Pittman DL, Williams AJK, et al. Islet autoantibody standardization program: Interlaboratory comparison of insulin autoantibody assay performance in 2018 and 2020 workshops[J]. Diabetologia, 2023, 66(5):897-912. doi:10.1007/s00125-023-05877-9.
pmid: 36759347 |
| [21] | 陈煦阳, 顾卫琼. 胰岛素自身抗体临床检测应用局限及对策研究进展[J]. 诊断学理论与实践, 2022, 21(1):95-98. doi:10.16150/j.1671-2870.2022.01.018. |
| [22] | 蒋雪松, 李佳. 外源性胰岛素自身免疫综合征合并线粒体糖尿病1例并文献复习[J]. 解放军医学院学报, 2024:1-5. |
| [23] |
Li R, Mao J, Yu K, et al. Medical nutrition therapy is effective in the management of hypoglycemia caused by insulin antibodies: A case report and literature review[J]. J Am Coll Nutr, 2016, 35(1):86-90. doi:10.1080/07315724.2014.976673.
pmid: 26273793 |
| [24] | Boro H, Gupta U, Singh C, et al. Continuous glucose monitoring and rituximab treatment in insulin autoimmune syndrome[J]. Diabetes Metab Syndr, 2021, 15(6):102294. doi:10.1016/j.dsx.2021.102294. |
| [25] | Monteiro SS, Santos TS, Dores J. Novel management of insulin autoimmune syndrome with methylprednisolone and flash glucose monitoring[J]. Ann Endocrinol (Paris), 2023, 84(1):83-85. doi:10.1016/j.ando.2022.10.001. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||