

临床荟萃 ›› 2025, Vol. 40 ›› Issue (9): 801-810.doi: 10.3969/j.issn.1004-583X.2025.09.005
收稿日期:2025-06-05
出版日期:2025-09-20
发布日期:2025-09-26
通讯作者:
邢广群
E-mail:xinggq@qdu.edu.cn
基金资助:
Chen Lu, Qi Xiaojing, Han Runhong, Xing Guangqun( )
)
Received:2025-06-05
Online:2025-09-20
Published:2025-09-26
Contact:
Xing Guangqun
E-mail:xinggq@qdu.edu.cn
摘要:
目的 分析抗中性粒细胞胞浆抗体(antineutrophil cytoplasmic antibody,ANCA)相关性血管炎(ANCA-associated vasculitis,AAV)患者贫血发生的原因,评价初始贫血程度、贫血类型及贫血治疗反应对判定AAV患者病情的价值及与肾脏预后和全因死亡率的关系。方法 本研究纳入2013-2022年在青岛大学附属医院确诊为AAV患者157例,根据初始就诊时的血红蛋白水平分为非贫血组、轻度贫血组、中重度贫血组,详细分析AAV贫血发生的原因,动态观察不同原因的贫血经治疗后的反应及变化特点,据初诊基线与随访终点的血红蛋白值高(H)低(L)变化,将患者分为HH、HL、LH、LL四组,对各组患者进行肾脏结局和全因死亡率分析。结果 符合纳入标准的157例AAV患者中,女性82例(52.2%),男性75例(47.8%),年龄20~86岁,中位年龄67岁。髓过氧化物酶(MPO)-ANCA阳性者137例,蛋白酶3(PR3)-ANCA阳性者18例,双阳性者2例。平均随访时间(37±30)个月。研究结束时28例进展为终末期肾功能衰竭,死亡31例。AAV初诊时贫血十分常见,仅11例无贫血,轻度贫血67例,中重度贫血79例。贫血原因前四位分别为炎症性贫血、肾性贫血、感染性贫血、心肾贫血综合征;单一原因贫血少见(9/146,6.16%),复合型贫血常见(137/146,93.84%)。致贫血原因累加数量越多,肾脏预后越差。据初诊基线与随访终点的血红蛋白值高(H)低(L)变化,肾脏结局和全因死亡率分析发现,HH组肾脏存活率最高,全因死亡率最低;LL组更易进展为终末期肾功能衰竭(P<0.05),全因死亡率最高(P<0.05)。结论 AAV中常见的贫血是AAV中活跃且有价值的系统判定病情及预后的监测指标,贫血发生与疾病活动性(BVAS评分)显著相关,复合原因贫血最多见。贫血治疗反应是肾功能恶化及全因死亡的独立预测因子。
中图分类号:
陈璐, 亓晓菁, 韩润鸿, 邢广群. 贫血在系统判定ANCA相关性小血管炎患者病情及预后中的作用[J]. 临床荟萃, 2025, 40(9): 801-810.
Chen Lu, Qi Xiaojing, Han Runhong, Xing Guangqun. The role of anemia in evaluating disease severity and prognosis of ANCA-associated vasculitis[J]. Clinical Focus, 2025, 40(9): 801-810.
| 贫血类型 | 诊断标准 |
|---|---|
| 缺铁性贫血 | 血清铁蛋白<10 μg/L(女)/<15 μg/L(男)或转铁蛋白饱和度<16%、血清铁蛋白<30 μg/L[ |
| 炎症性贫血 | 血清铁低、转铁蛋白饱和度<20%、铁蛋白>100 μg/L、CRP/红细胞沉降率(erythrocyte sedimentation rate, ESR)升高、正常细胞正色素性贫血[ |
| 肾性贫血 | 肾功能下降、促红细胞生成素减少、红细胞寿命缩短[ |
| 感染性贫血 | 临床/实验室/影像学证据支持的感染,伴抗生素治疗。 |
| 心肾贫血综合征 | 心力衰竭、估算肾小球滤过率(estimated glomerular filtration rate,eGFR)<60 ml/(min·1.73m2)、HGB<130 g/L(男)或<120 g/L(女) [ |
| 叶酸缺乏性贫血 | 血清叶酸<3 μg/L[ |
表1 贫血原因分类
Tab.1 Classification of causes of anemia
| 贫血类型 | 诊断标准 |
|---|---|
| 缺铁性贫血 | 血清铁蛋白<10 μg/L(女)/<15 μg/L(男)或转铁蛋白饱和度<16%、血清铁蛋白<30 μg/L[ |
| 炎症性贫血 | 血清铁低、转铁蛋白饱和度<20%、铁蛋白>100 μg/L、CRP/红细胞沉降率(erythrocyte sedimentation rate, ESR)升高、正常细胞正色素性贫血[ |
| 肾性贫血 | 肾功能下降、促红细胞生成素减少、红细胞寿命缩短[ |
| 感染性贫血 | 临床/实验室/影像学证据支持的感染,伴抗生素治疗。 |
| 心肾贫血综合征 | 心力衰竭、估算肾小球滤过率(estimated glomerular filtration rate,eGFR)<60 ml/(min·1.73m2)、HGB<130 g/L(男)或<120 g/L(女) [ |
| 叶酸缺乏性贫血 | 血清叶酸<3 μg/L[ |
| 项目 | 非贫血组 | 轻度贫血组 | 中重度贫血组 | ||
|---|---|---|---|---|---|
| 例数 | 11 | 67 | 79 | ||
| 男/女 | 5/6 | 35/32 | 35/44 | 0.940 | 0.625 |
| 年龄(岁) | 64.0(53.0, 71.0) | 68.0(60.0, 75.0) | 67.0(60.0, 72.0) | 1.792 | 0.408 |
| 初诊HGB(g/L) | 133.00±12.78 | 104.63±10.93 | 72.65±10.19 | 255.490 | <0.01 |
| MCV(fl) | 90.19±2.59 | 89.72±5.29 | 89.68±5.44 | 0.046 | 0.955 |
| MCH(pg) | 30.05±0.76 | 29.27±1.82 | 29.25±2.16 | 2.841 | 0.242 |
| MCHC(g/L) | 333.27±9.48 | 326.51±16.58 | 326.13±15.70 | 1.011 | 0.366 |
| CRP(mg/L) | 1.51(0.66, 9.79) | 17.67(0.96, 80.43) | 52.30(7.61, 101.08) | 10.120 | 0.006 |
| ESR(mm/h) | 14.85(11.33, 21.00) | 49.00(23.40, 84.40) | 86.40(42.70, 108.00) | 24.367 | <0.01 |
| SCr(μmol/L) | 97.00(82.30, 126.70) | 153.45(95.63, 311.98) | 542.20(297.50, 784.10) | 48.923 | <0.01 |
| eGFR[ml/(min·1.73 m2)] | 64.68(40.59, 73.54) | 32.52(16.39, 54.39) | 9.56(6.09, 18.53) | 49.006 | <0.01 |
| BUN(mmol/L) | 5.42(4.78, 8.10) | 9.84(6.69, 17.49) | 26.50(17.70, 37.45) | 55.572 | <0.01 |
| UA(mmol/L) | 338.22±47.98 | 382.61±167.98 | 454.90±153.51 | 9.911 | 0.007 |
| ALB(g/L) | 36.83±7.34 | 32.32±5.34 | 29.33±5.22 | 11.445 | <0.01 |
| DD( μg/L) | 270.00(96.25, 530.00) | 465.00(257.50, 1062.00) | 1410.00(562.00, 3570.00) | 34.510 | <0.01 |
| 24 h尿蛋白定量(g/24 h) | 0.91(0.44, 2.34) | 1.09(0.30, 1.89) | 1.11(0.72, 2.47) | 1.701 | 0.427 |
| 尿常规红细胞数(个/μl) | 105.15(12.39, 388.48) | 63.65(19.62, 250.58) | 187.44(48.50, 687.10) | 9.675 | 0.008 |
| PCT(μg/L) | 0.13(0.06, 0.20) | 0.13(0.07, 0.33) | 0.32(0.16, 0.70) | 14.040 | 0.001 |
| CD4绝对计数(cells/μl) | 568.00(469.25, 726.00) | 478.00(334.00, 806.00) | 381.00(183.00, 639.00) | 6.069 | 0.048 |
| C3(g/L) | 1.04(0.95, 1.22) | 1.03(0.87, 1.23) | 0.91(0.77, 1.02) | 11.788 | 0.003 |
| C4(g/L) | 0.29±0.08 | 0.26±0.10 | 0.23±0.08 | 3.084 | 0.049 |
| BNP(ng/L) | 101.35(18.50, 670.28) | 78.90(42.50, 180.50) | 263.30(103.40, 847.60) | 11.246 | 0.004 |
| Hs-TnI(μg/L) | 0.004(0.002, 0.018) | 0.006(0.003, 0.012) | 0.016(0.009, 0.047) | 13.774 | 0.001 |
| EF% | 62.00(60.50, 64.50) | 63.00(61.00, 64.00) | 62.00(58.00, 63.00) | 5.139 | 0.077 |
| 叶酸(μg/L) | 6.99(5.26, 7.64) | 5.13(3.73, 9.64) | 5.00(3.05, 12.69) | 0.347 | 0.841 |
| 维生素B12(ng/L) | 1008.76(598.86, 1815.75) | 590.37(430.23, 1028.73) | 547.62(356.50, 957.08) | 3.153 | 0.207 |
| 结合珠蛋白(g/L) | 1.66(1.08, 3.21) | 2.02(0.95, 3.03) | 1.74(1.17, 2.60) | 0.050 | 0.975 |
| 铁蛋白(μg/L) | 327.00(60.60, 759.10) | 329.60(198.00, 704.22) | 436.04(203.50, 737.44) | 2.080 | 0.353 |
| 转铁蛋白(g/L) | 1.33±0.58 | 1.60±0.50 | 1.40±0.39 | 2.092 | 0.130 |
| 可溶性转铁蛋白受体(mg/L) | 0.64(0.39, 1.41) | 1.11(0.91, 1.31) | 0.87(0.64, 1.05) | 8.624 | 0.013 |
| BVAS | 13.36±5.82 | 14.61±5.36 | 18.87±5.61 | 12.927 | <0.01 |
| FFS | 1.00(1.00, 2.00) | 2.00(2.00, 3.00) | 3.00(2.00, 3.00) | 11.600 | 0.003 |
| CCI | 1.00(1.00, 2.00) | 2.00(1.00, 3.00) | 4.00(3.00, 4.00) | 40.413 | <0.01 |
表2 初诊时不同HGB水平AAV患者的临床资料及基线特征
Tab.2 Clinical data and baseline characteristics of AAV patients with different HGB levels at the initial diagnosis
| 项目 | 非贫血组 | 轻度贫血组 | 中重度贫血组 | ||
|---|---|---|---|---|---|
| 例数 | 11 | 67 | 79 | ||
| 男/女 | 5/6 | 35/32 | 35/44 | 0.940 | 0.625 |
| 年龄(岁) | 64.0(53.0, 71.0) | 68.0(60.0, 75.0) | 67.0(60.0, 72.0) | 1.792 | 0.408 |
| 初诊HGB(g/L) | 133.00±12.78 | 104.63±10.93 | 72.65±10.19 | 255.490 | <0.01 |
| MCV(fl) | 90.19±2.59 | 89.72±5.29 | 89.68±5.44 | 0.046 | 0.955 |
| MCH(pg) | 30.05±0.76 | 29.27±1.82 | 29.25±2.16 | 2.841 | 0.242 |
| MCHC(g/L) | 333.27±9.48 | 326.51±16.58 | 326.13±15.70 | 1.011 | 0.366 |
| CRP(mg/L) | 1.51(0.66, 9.79) | 17.67(0.96, 80.43) | 52.30(7.61, 101.08) | 10.120 | 0.006 |
| ESR(mm/h) | 14.85(11.33, 21.00) | 49.00(23.40, 84.40) | 86.40(42.70, 108.00) | 24.367 | <0.01 |
| SCr(μmol/L) | 97.00(82.30, 126.70) | 153.45(95.63, 311.98) | 542.20(297.50, 784.10) | 48.923 | <0.01 |
| eGFR[ml/(min·1.73 m2)] | 64.68(40.59, 73.54) | 32.52(16.39, 54.39) | 9.56(6.09, 18.53) | 49.006 | <0.01 |
| BUN(mmol/L) | 5.42(4.78, 8.10) | 9.84(6.69, 17.49) | 26.50(17.70, 37.45) | 55.572 | <0.01 |
| UA(mmol/L) | 338.22±47.98 | 382.61±167.98 | 454.90±153.51 | 9.911 | 0.007 |
| ALB(g/L) | 36.83±7.34 | 32.32±5.34 | 29.33±5.22 | 11.445 | <0.01 |
| DD( μg/L) | 270.00(96.25, 530.00) | 465.00(257.50, 1062.00) | 1410.00(562.00, 3570.00) | 34.510 | <0.01 |
| 24 h尿蛋白定量(g/24 h) | 0.91(0.44, 2.34) | 1.09(0.30, 1.89) | 1.11(0.72, 2.47) | 1.701 | 0.427 |
| 尿常规红细胞数(个/μl) | 105.15(12.39, 388.48) | 63.65(19.62, 250.58) | 187.44(48.50, 687.10) | 9.675 | 0.008 |
| PCT(μg/L) | 0.13(0.06, 0.20) | 0.13(0.07, 0.33) | 0.32(0.16, 0.70) | 14.040 | 0.001 |
| CD4绝对计数(cells/μl) | 568.00(469.25, 726.00) | 478.00(334.00, 806.00) | 381.00(183.00, 639.00) | 6.069 | 0.048 |
| C3(g/L) | 1.04(0.95, 1.22) | 1.03(0.87, 1.23) | 0.91(0.77, 1.02) | 11.788 | 0.003 |
| C4(g/L) | 0.29±0.08 | 0.26±0.10 | 0.23±0.08 | 3.084 | 0.049 |
| BNP(ng/L) | 101.35(18.50, 670.28) | 78.90(42.50, 180.50) | 263.30(103.40, 847.60) | 11.246 | 0.004 |
| Hs-TnI(μg/L) | 0.004(0.002, 0.018) | 0.006(0.003, 0.012) | 0.016(0.009, 0.047) | 13.774 | 0.001 |
| EF% | 62.00(60.50, 64.50) | 63.00(61.00, 64.00) | 62.00(58.00, 63.00) | 5.139 | 0.077 |
| 叶酸(μg/L) | 6.99(5.26, 7.64) | 5.13(3.73, 9.64) | 5.00(3.05, 12.69) | 0.347 | 0.841 |
| 维生素B12(ng/L) | 1008.76(598.86, 1815.75) | 590.37(430.23, 1028.73) | 547.62(356.50, 957.08) | 3.153 | 0.207 |
| 结合珠蛋白(g/L) | 1.66(1.08, 3.21) | 2.02(0.95, 3.03) | 1.74(1.17, 2.60) | 0.050 | 0.975 |
| 铁蛋白(μg/L) | 327.00(60.60, 759.10) | 329.60(198.00, 704.22) | 436.04(203.50, 737.44) | 2.080 | 0.353 |
| 转铁蛋白(g/L) | 1.33±0.58 | 1.60±0.50 | 1.40±0.39 | 2.092 | 0.130 |
| 可溶性转铁蛋白受体(mg/L) | 0.64(0.39, 1.41) | 1.11(0.91, 1.31) | 0.87(0.64, 1.05) | 8.624 | 0.013 |
| BVAS | 13.36±5.82 | 14.61±5.36 | 18.87±5.61 | 12.927 | <0.01 |
| FFS | 1.00(1.00, 2.00) | 2.00(2.00, 3.00) | 3.00(2.00, 3.00) | 11.600 | 0.003 |
| CCI | 1.00(1.00, 2.00) | 2.00(1.00, 3.00) | 4.00(3.00, 4.00) | 40.413 | <0.01 |
| 项目 | 炎症性贫血( | 肾性贫血( | 感染性贫血( | 心肾贫血综合征( | 叶酸缺乏所致贫血( | 缺铁性贫血( | 失血性贫血( |
|---|---|---|---|---|---|---|---|
| 人数[例(%)] | 146(100.0) | 133(91.1) | 61(41.8) | 40(27.4) | 16(11.0) | 11(7.5) | 8(5.4) |
| 年龄(岁) | 67.50(60.00, 74.00) | 68.00(60.00, 74.00) | 68.00(63.50, 75.00) | 69.50(63.25, 79.50) | 69.50(59.50, 80.75) | 65.00(47.00, 74.00) | 64.00(43.75, 70.50) |
| 初诊HGB(g/L) | 86.00(71.00, 101.25) | 85.00(70.00, 98.50) | 87.00(70.00, 101.50) | 81.50(66.00, 86.75) | 69.00(60.50, 84.50) | 85.00(74.00, 103.00) | 79.50(54.75, 92.00) |
| MCV(fl) | 90.60(87.95, 93.28) | 88.70(85.25, 93.55) | 87.60(85.10, 92.70) | 90.80(86.68, 94.93) | 86.45(84.60, 90.50) | 87.40(82.80, 91.20) | 91.05(89.15, 94.65) |
| MCH(pg) | 29.45(28.68, 29.75) | 29.30(27.85, 30.60) | 28.30(27.25, 30.10) | 29.70(27.35, 30.65) | 28.90(27.75, 30.08) | 29.00(26.30, 29.60) | 29.80(28.50, 30.38) |
| MCHC(g/L) | 324.50(314.50, 332.50) | 328.00(317.00, 336.50) | 324.00(309.50, 334.50) | 325.50(313.50, 335.00) | 327.50(322.50, 338.75) | 322.00(310.00, 335.00) | 325.50(318.25, 327.50) |
| CRP(mg/L) | 36.02(3.66, 97.84) | 28.27(3.02, 98.64) | 69.58(15.31, 129.88) | 36.41(6.31, 109.15) | 91.17(20.32, 151.06) | 13.56(2.18, 69.58) | 21.41(2.37, 126.99) |
| ESR(mm/h) | 72.00(27.68, 99.25) | 74.30(27.45,100.00) | 75.10(37.15, 107.00) | 55.15(21.40, 99.00) | 49.00(30.43, 96.28) | 27.00(12.00, 78.80) | 39.35(24.33, 98.25) |
| SCr(μmol/L) | 311.00(146.05, 655.70) | 364.75(167.45, 691.23) | 394.90(163.80, 671.95) | 650.20(352.00, 822.70) | 705.75(530.95, 975.38) | 328.30(146.80, 980.00) | 341.20(271.58, 713.80) |
| eGFR[ml/(min·1.73 m2)] | 16.72(7.91, 33.74) | 14.71(7.30, 28.28) | 13.94(6.22, 27.18) | 8.77(5.50, 14.71) | 8.32(5.09, 11.52) | 12.41(5.51, 35.88) | 15.72(9.01, 27.34) |
| BUN(mmol/L) | 19.20(9.19, 29.79) | 19.93(11.38, 30.93) | 20.00(10.56, 31.75) | 29.93(19.58, 42.43) | 30.35(22.63, 48.11) | 20.00(13.01, 26.59) | 20.04(15.22, 32.35) |
| UA(mmol/L) | 423.20(282.50, 525.88) | 439.00(304.40, 563.00) | 392.80(282.85, 515.70) | 472.70(370.35, 637.30) | 420.05(275.73, 573.58) | 534.70(291.40, 653.00) | 472.30(279.00, 534.70) |
| ALB(g/L) | 31.10(26.90, 34.50) | 30.70(26.41,34.50) | 29.70(25.50, 33.90) | 28.42(24.42, 33.70) | 28.15(24.01, 30.47) | 32.60(29.70, 34.20) | 32.95(26.40, 35.60) |
| DD(μg/L) | 780.00(354.00, 2280.00) | 820.00(352.00, 2367.50) | 859.50(295.75, 1840.00) | 1410.00(720.00, 4970.00) | 2225.00(1457.50, 5980.00) | 470.00(207.00, 1141.00) | 2099.00(450.25, 5622.50) |
| 24 h尿蛋白定量(g/24 h) | 1.11(0.62, 2.08) | 1.11(0.63, 2.08) | 0.72(0.31, 1.48) | 1.30(0.63, 2.80) | 1.79(0.72, 4.01) | 0.86(0.22, 2.13) | 0.89(0.63, 1.23) |
| 尿常规红细胞数(个/μl) | 122.30(30.50, 396.20) | 123.40(31.48, 444.20) | 79.20(33.60, 227.00) | 91.00(31.80, 285.00) | 188.00(48.18, 559.10) | 228.00(69.80, 489.15) | 228.00(26.00, 395.00) |
| PCT(μg/L) | 0.24(0.11, 0.60) | 0.25(0.12, 0.63) | 0.40(0.13, 0.94) | 0.51(0.20, 0.89) | 0.57(0.32, 0.94) | 0.33(0.29, 1.62) | 0.25(0.16, 0.34) |
| C3(g/L) | 0.95(0.81, 1.09) | 0.95(0.80, 1.07) | 0.97(0.80, 1.18) | 0.88(0.64, 0.96) | 0.84(0.76, 1.03) | 1.00(0.70, 1.15) | 0.86(0.62, 1.11) |
| C4(g/L) | 0.24(0.19, 0.29) | 0.24(0.18, 0.29) | 0.23(0.16, 0.29) | 0.20(0.17, 0.27) | 0.20(0.14, 0.29) | 0.21(0.18, 0.25) | 0.19(0.15,0.24) |
| BNP(ng/L) | 159.70(54.58, 644.03) | 181.70(62.53, 666.83) | 258.75(72.03, 1079.60) | 884.90(292.80, 1528.15) | 263.00(114.55, 617.03) | 180.50(103.40, 652.20) | 263.30(77.8, 1895.1) |
| Hs-TnI(μg/L) | 0.012(0.005, 0.042) | 0.014(0.006, 0.043) | 0.021(0.007, 0.066) | 0.037(0.012, 0.089) | 0.021(0.008, 0.059) | 0.012(0.004, 0.032) | 0.026(0.004, 0.160) |
| EF% | 62.00(60.00, 63.00) | 62.00(60.00, 63.00) | 62.00(60.00, 64.75) | 60.00(56.00, 62.00) | 62.00(60.00, 63.00) | 63.00(61.00, 65.00) | 66.00(60.00, 67.00) |
| 叶酸(μg/L) | 5.01(3.13, 11.89) | 5.01(3.10, 11.89) | 6.42(2.57, 12.85) | 7.72(2.84, 17.02) | 2.09(1.48, 2.55) | 10.03(3.51, 19.53) | 2.52(1.51, 6.57) |
| 维生素B12(ng/L) | 551.63(361.03, 981.50) | 547.62(358.75, 1016.73) | 677.68(404.65, 1150.90) | 677.68(384.77, 1069.51) | 687.29(305.46, 1144.62) | 648.79(424.54, 1690.57) | 316.29(245.81, 502.65) |
| 结合珠蛋白(g/L) | 1.83(1.12, 2.64) | 1.74(1.08, 2.63) | 1.85(1.15, 2.78) | 1.76(1.15, 2.57) | 1.45(0.66, 2.90) | 1.29(0.93, 2.28) | 1.64(1.41, 3.45) |
| 铁蛋白(μg/L) | 397.65(204.33, 708.26) | 386.58(202.65, 715.99) | 484.02(191.02, 901.44) | 614.35(197.72, 1004.93) | 964.50(425.48, 1307.00) | 68.58(23.87, 92.82) | 187.99(124.84, 1071.75) |
| 转铁蛋白(g/L) | 1.45(1.17, 1.72) | 1.46(1.17, 1.74) | 1.33(1.09, 1.56) | 1.25(0.94, 1.55) | 1.21(0.90, 1.46) | 1.82(1.71, 2.44) | 1.61(1.30, 1.72) |
| 可溶性转铁蛋白受体(mg/L) | 0.93(0.70, 1.22) | 0.92(0.70, 1.22) | 0.86(0.63, 1.07) | 0.89(0.64, 1.14) | 0.76(0.60, 0.90) | 1.21(0.98, 1.79) | 0.85(0.78, 0.93) |
| BVAS | 16.92±5.88 | 17.28±5.85 | 18.11±5.51 | 20.93±5.37 | 20.50±5.54 | 16.18±6.03 | 20.75±7.74 |
| FFS | 2.47±0.96 | 2.56±0.91 | 2.66±0.93 | 3.30±0.72 | 2.88±0.96 | 2.36±1.21 | 2.63±0.92 |
| CCI | 3.09±1.36 | 3.19±1.35 | 3.43±1.35 | 4.13±0.97 | 3.69±0.79 | 3.45±1.21 | 3.88±0.64 |
表3 不同贫血原因AAV患者的临床特征比较
Tab.3 Comparison of clinical characteristics of AAV patients with different causes of anemia
| 项目 | 炎症性贫血( | 肾性贫血( | 感染性贫血( | 心肾贫血综合征( | 叶酸缺乏所致贫血( | 缺铁性贫血( | 失血性贫血( |
|---|---|---|---|---|---|---|---|
| 人数[例(%)] | 146(100.0) | 133(91.1) | 61(41.8) | 40(27.4) | 16(11.0) | 11(7.5) | 8(5.4) |
| 年龄(岁) | 67.50(60.00, 74.00) | 68.00(60.00, 74.00) | 68.00(63.50, 75.00) | 69.50(63.25, 79.50) | 69.50(59.50, 80.75) | 65.00(47.00, 74.00) | 64.00(43.75, 70.50) |
| 初诊HGB(g/L) | 86.00(71.00, 101.25) | 85.00(70.00, 98.50) | 87.00(70.00, 101.50) | 81.50(66.00, 86.75) | 69.00(60.50, 84.50) | 85.00(74.00, 103.00) | 79.50(54.75, 92.00) |
| MCV(fl) | 90.60(87.95, 93.28) | 88.70(85.25, 93.55) | 87.60(85.10, 92.70) | 90.80(86.68, 94.93) | 86.45(84.60, 90.50) | 87.40(82.80, 91.20) | 91.05(89.15, 94.65) |
| MCH(pg) | 29.45(28.68, 29.75) | 29.30(27.85, 30.60) | 28.30(27.25, 30.10) | 29.70(27.35, 30.65) | 28.90(27.75, 30.08) | 29.00(26.30, 29.60) | 29.80(28.50, 30.38) |
| MCHC(g/L) | 324.50(314.50, 332.50) | 328.00(317.00, 336.50) | 324.00(309.50, 334.50) | 325.50(313.50, 335.00) | 327.50(322.50, 338.75) | 322.00(310.00, 335.00) | 325.50(318.25, 327.50) |
| CRP(mg/L) | 36.02(3.66, 97.84) | 28.27(3.02, 98.64) | 69.58(15.31, 129.88) | 36.41(6.31, 109.15) | 91.17(20.32, 151.06) | 13.56(2.18, 69.58) | 21.41(2.37, 126.99) |
| ESR(mm/h) | 72.00(27.68, 99.25) | 74.30(27.45,100.00) | 75.10(37.15, 107.00) | 55.15(21.40, 99.00) | 49.00(30.43, 96.28) | 27.00(12.00, 78.80) | 39.35(24.33, 98.25) |
| SCr(μmol/L) | 311.00(146.05, 655.70) | 364.75(167.45, 691.23) | 394.90(163.80, 671.95) | 650.20(352.00, 822.70) | 705.75(530.95, 975.38) | 328.30(146.80, 980.00) | 341.20(271.58, 713.80) |
| eGFR[ml/(min·1.73 m2)] | 16.72(7.91, 33.74) | 14.71(7.30, 28.28) | 13.94(6.22, 27.18) | 8.77(5.50, 14.71) | 8.32(5.09, 11.52) | 12.41(5.51, 35.88) | 15.72(9.01, 27.34) |
| BUN(mmol/L) | 19.20(9.19, 29.79) | 19.93(11.38, 30.93) | 20.00(10.56, 31.75) | 29.93(19.58, 42.43) | 30.35(22.63, 48.11) | 20.00(13.01, 26.59) | 20.04(15.22, 32.35) |
| UA(mmol/L) | 423.20(282.50, 525.88) | 439.00(304.40, 563.00) | 392.80(282.85, 515.70) | 472.70(370.35, 637.30) | 420.05(275.73, 573.58) | 534.70(291.40, 653.00) | 472.30(279.00, 534.70) |
| ALB(g/L) | 31.10(26.90, 34.50) | 30.70(26.41,34.50) | 29.70(25.50, 33.90) | 28.42(24.42, 33.70) | 28.15(24.01, 30.47) | 32.60(29.70, 34.20) | 32.95(26.40, 35.60) |
| DD(μg/L) | 780.00(354.00, 2280.00) | 820.00(352.00, 2367.50) | 859.50(295.75, 1840.00) | 1410.00(720.00, 4970.00) | 2225.00(1457.50, 5980.00) | 470.00(207.00, 1141.00) | 2099.00(450.25, 5622.50) |
| 24 h尿蛋白定量(g/24 h) | 1.11(0.62, 2.08) | 1.11(0.63, 2.08) | 0.72(0.31, 1.48) | 1.30(0.63, 2.80) | 1.79(0.72, 4.01) | 0.86(0.22, 2.13) | 0.89(0.63, 1.23) |
| 尿常规红细胞数(个/μl) | 122.30(30.50, 396.20) | 123.40(31.48, 444.20) | 79.20(33.60, 227.00) | 91.00(31.80, 285.00) | 188.00(48.18, 559.10) | 228.00(69.80, 489.15) | 228.00(26.00, 395.00) |
| PCT(μg/L) | 0.24(0.11, 0.60) | 0.25(0.12, 0.63) | 0.40(0.13, 0.94) | 0.51(0.20, 0.89) | 0.57(0.32, 0.94) | 0.33(0.29, 1.62) | 0.25(0.16, 0.34) |
| C3(g/L) | 0.95(0.81, 1.09) | 0.95(0.80, 1.07) | 0.97(0.80, 1.18) | 0.88(0.64, 0.96) | 0.84(0.76, 1.03) | 1.00(0.70, 1.15) | 0.86(0.62, 1.11) |
| C4(g/L) | 0.24(0.19, 0.29) | 0.24(0.18, 0.29) | 0.23(0.16, 0.29) | 0.20(0.17, 0.27) | 0.20(0.14, 0.29) | 0.21(0.18, 0.25) | 0.19(0.15,0.24) |
| BNP(ng/L) | 159.70(54.58, 644.03) | 181.70(62.53, 666.83) | 258.75(72.03, 1079.60) | 884.90(292.80, 1528.15) | 263.00(114.55, 617.03) | 180.50(103.40, 652.20) | 263.30(77.8, 1895.1) |
| Hs-TnI(μg/L) | 0.012(0.005, 0.042) | 0.014(0.006, 0.043) | 0.021(0.007, 0.066) | 0.037(0.012, 0.089) | 0.021(0.008, 0.059) | 0.012(0.004, 0.032) | 0.026(0.004, 0.160) |
| EF% | 62.00(60.00, 63.00) | 62.00(60.00, 63.00) | 62.00(60.00, 64.75) | 60.00(56.00, 62.00) | 62.00(60.00, 63.00) | 63.00(61.00, 65.00) | 66.00(60.00, 67.00) |
| 叶酸(μg/L) | 5.01(3.13, 11.89) | 5.01(3.10, 11.89) | 6.42(2.57, 12.85) | 7.72(2.84, 17.02) | 2.09(1.48, 2.55) | 10.03(3.51, 19.53) | 2.52(1.51, 6.57) |
| 维生素B12(ng/L) | 551.63(361.03, 981.50) | 547.62(358.75, 1016.73) | 677.68(404.65, 1150.90) | 677.68(384.77, 1069.51) | 687.29(305.46, 1144.62) | 648.79(424.54, 1690.57) | 316.29(245.81, 502.65) |
| 结合珠蛋白(g/L) | 1.83(1.12, 2.64) | 1.74(1.08, 2.63) | 1.85(1.15, 2.78) | 1.76(1.15, 2.57) | 1.45(0.66, 2.90) | 1.29(0.93, 2.28) | 1.64(1.41, 3.45) |
| 铁蛋白(μg/L) | 397.65(204.33, 708.26) | 386.58(202.65, 715.99) | 484.02(191.02, 901.44) | 614.35(197.72, 1004.93) | 964.50(425.48, 1307.00) | 68.58(23.87, 92.82) | 187.99(124.84, 1071.75) |
| 转铁蛋白(g/L) | 1.45(1.17, 1.72) | 1.46(1.17, 1.74) | 1.33(1.09, 1.56) | 1.25(0.94, 1.55) | 1.21(0.90, 1.46) | 1.82(1.71, 2.44) | 1.61(1.30, 1.72) |
| 可溶性转铁蛋白受体(mg/L) | 0.93(0.70, 1.22) | 0.92(0.70, 1.22) | 0.86(0.63, 1.07) | 0.89(0.64, 1.14) | 0.76(0.60, 0.90) | 1.21(0.98, 1.79) | 0.85(0.78, 0.93) |
| BVAS | 16.92±5.88 | 17.28±5.85 | 18.11±5.51 | 20.93±5.37 | 20.50±5.54 | 16.18±6.03 | 20.75±7.74 |
| FFS | 2.47±0.96 | 2.56±0.91 | 2.66±0.93 | 3.30±0.72 | 2.88±0.96 | 2.36±1.21 | 2.63±0.92 |
| CCI | 3.09±1.36 | 3.19±1.35 | 3.43±1.35 | 4.13±0.97 | 3.69±0.79 | 3.45±1.21 | 3.88±0.64 |
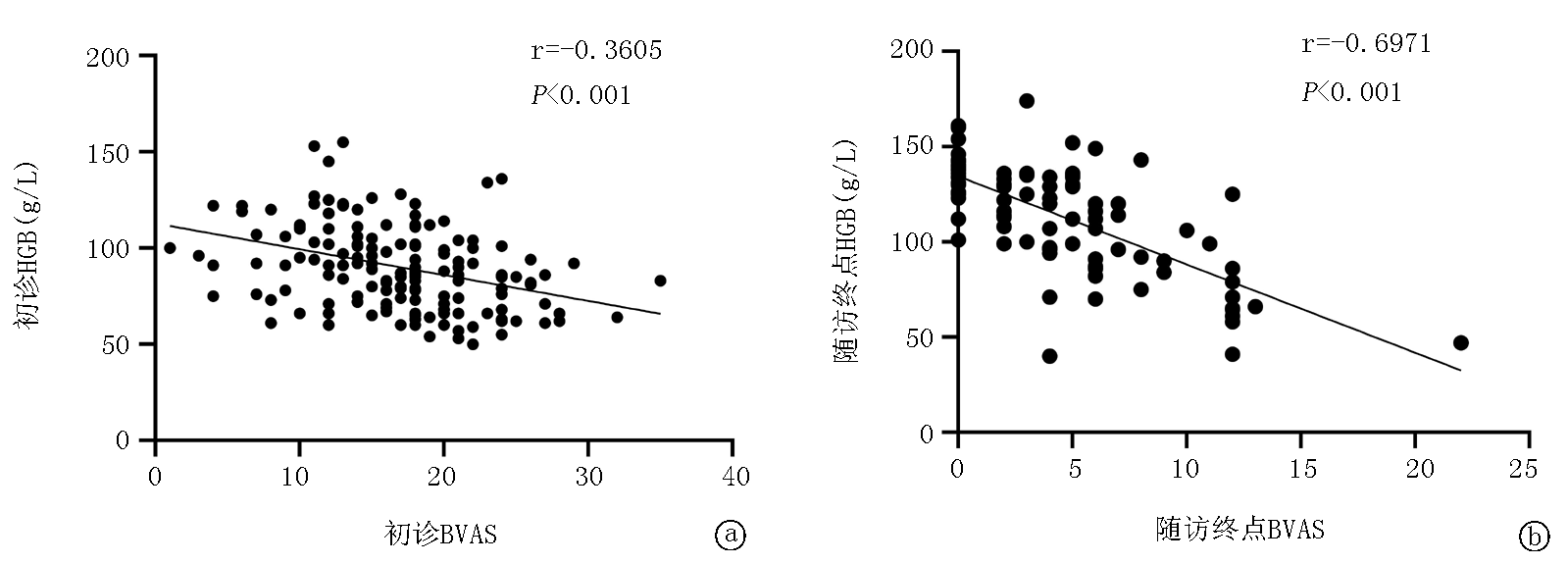
图3 HGB与BVAS评分的相关性分析 a.初始HGB与初始BVAS评分的相关性分析;b.终点HGB与终点BVAS评分的相关性分析
Fig.3 Correlation analysis of HGB and BVAS scores a.Correlation analysis between initial HGB and initial BVAS score; b.Correlation analysis of end-point HGB and end-point BVAS score
| 项目 | HH( | HL( | LH( | LL( | ||
|---|---|---|---|---|---|---|
| 年龄(岁) | 67.00(65.25, 72.25) | 67.00(59.75, 71.50) | 71.00(65.00, 76.00) | 67.00(57.00, 75.00) | 3.470 | 0.325 |
| 初诊HGB(g/L) | 123.00(118.25, 133.75) | 112.00(110.75, 120.50) | 91.00(78.50, 99.50)*△ | 80.50(68.00, 93.75)*△ | 53.621 | <0.01 |
| 末次HGB(g/L) | 142.00±14.50 | 81.17±21.52* | 127.98±10.28*△ | 83.16±19.00*# | 80.015 | <0.01 |
| 末次CRP(mg/L) | 1.30(0.50, 2.97) | 71.33(21.90, 94.85)* | 1.10(0.50, 4.17)△ | 5.16(0.54, 26.49) | 16.984 | 0.001 |
| 末次ESR(mm/h) | 12.85(7.10, 15.05) | 110.00(104.25, 118.00)* | 15.30(10.10, 22.00)△ | 24.00(15.58, 68.90) | 19.026 | <0.01 |
| 末次SCr(μmol/L) | 106.00(82.20, 118.90) | 361.60(259.08, 907.10)* | 122.20(101.80, 158.75)△ | 298.70(185.53, 538.63)*# | 42.187 | <0.01 |
| 末次eGFR[(ml/(min·1.73 m2)] | 61.44(42.42, 65.56) | 13.46(7.26, 16.81)* | 37.47(26.29, 49.81)△ | 12.94(7.95, 27.65)*# | 43.276 | <0.01 |
| 末次BUN(mmol/L) | 5.48(4.81, 8.51) | 25.14(20.56, 49.77)* | 9.76(6.78, 14.21)*△ | 24.50(13.33, 39.10)*# | 46.244 | <0.01 |
| 末次UA(mmol/L) | 338.10(258.70, 462.70) | 526.85(397.48, 631.75) | 393.50(301.20, 478.98) | 379.00(251.00, 651.10) | 4.979 | 0.173 |
| 末次ALB(g/L) | 40.91(40.10, 42.90) | 26.50(21.33, 31.28)* | 38.75(36.15, 40.70)△ | 32.80(28.90, 36.40)*# | 34.382 | <0.01 |
| 末次BVAS | 2.50(0.00, 3.75) | 10.50(7.50, 14.50)* | 2.00(0.00, 5.00)△ | 6.00(4.00, 11.75)*# | 34.586 | <0.01 |
| 末次FFS | 1.00(1.00, 1.00) | 2.00(1.00, 3.00) | 1.00(1.00, 2.00) | 1.50(1.00, 2.00) | 9.104 | 0.028 |
表4 根据HGB初诊基线和随访终点动态变化分组的AAV患者随访终点特征比较
Tab.4 Comparison of follow-up endpoint characteristics of AAV patients grouped by the dynamic changes of HGB at initial diagnosis baseline and follow-up endpoint
| 项目 | HH( | HL( | LH( | LL( | ||
|---|---|---|---|---|---|---|
| 年龄(岁) | 67.00(65.25, 72.25) | 67.00(59.75, 71.50) | 71.00(65.00, 76.00) | 67.00(57.00, 75.00) | 3.470 | 0.325 |
| 初诊HGB(g/L) | 123.00(118.25, 133.75) | 112.00(110.75, 120.50) | 91.00(78.50, 99.50)*△ | 80.50(68.00, 93.75)*△ | 53.621 | <0.01 |
| 末次HGB(g/L) | 142.00±14.50 | 81.17±21.52* | 127.98±10.28*△ | 83.16±19.00*# | 80.015 | <0.01 |
| 末次CRP(mg/L) | 1.30(0.50, 2.97) | 71.33(21.90, 94.85)* | 1.10(0.50, 4.17)△ | 5.16(0.54, 26.49) | 16.984 | 0.001 |
| 末次ESR(mm/h) | 12.85(7.10, 15.05) | 110.00(104.25, 118.00)* | 15.30(10.10, 22.00)△ | 24.00(15.58, 68.90) | 19.026 | <0.01 |
| 末次SCr(μmol/L) | 106.00(82.20, 118.90) | 361.60(259.08, 907.10)* | 122.20(101.80, 158.75)△ | 298.70(185.53, 538.63)*# | 42.187 | <0.01 |
| 末次eGFR[(ml/(min·1.73 m2)] | 61.44(42.42, 65.56) | 13.46(7.26, 16.81)* | 37.47(26.29, 49.81)△ | 12.94(7.95, 27.65)*# | 43.276 | <0.01 |
| 末次BUN(mmol/L) | 5.48(4.81, 8.51) | 25.14(20.56, 49.77)* | 9.76(6.78, 14.21)*△ | 24.50(13.33, 39.10)*# | 46.244 | <0.01 |
| 末次UA(mmol/L) | 338.10(258.70, 462.70) | 526.85(397.48, 631.75) | 393.50(301.20, 478.98) | 379.00(251.00, 651.10) | 4.979 | 0.173 |
| 末次ALB(g/L) | 40.91(40.10, 42.90) | 26.50(21.33, 31.28)* | 38.75(36.15, 40.70)△ | 32.80(28.90, 36.40)*# | 34.382 | <0.01 |
| 末次BVAS | 2.50(0.00, 3.75) | 10.50(7.50, 14.50)* | 2.00(0.00, 5.00)△ | 6.00(4.00, 11.75)*# | 34.586 | <0.01 |
| 末次FFS | 1.00(1.00, 1.00) | 2.00(1.00, 3.00) | 1.00(1.00, 2.00) | 1.50(1.00, 2.00) | 9.104 | 0.028 |
| 项目 | 回归系数 | 标准误 | Wald χ2值 | 风险比 | 95% | |
|---|---|---|---|---|---|---|
| 年龄 | -0.008 | 0.011 | 0.553 | 0.992 | 0.970~1.014 | 0.457 |
| 初诊HGB(g/L) | -0.025 | 0.008 | 9.874 | 0.975 | 0.960~0.991 | 0.002 |
| CRP(mg/L) | -0.002 | 0.003 | 0.455 | 0.998 | 0.992~1.004 | 0.500 |
| ESR(mm/h) | 0.003 | 0.004 | 0.623 | 1.003 | 0.996~1.010 | 0.430 |
| SCr(μmol/L) | 0.001 | 0 | 12.405 | 1.001 | 1.001~1.002 | <0.01 |
| eGFR[ml/(min·1.73 m2)] | -0.031 | 0.009 | 11.497 | 0.97 | 0.952~0.987 | 0.001 |
| BUN(mmol/L) | 0.030 | 0.008 | 14.352 | 1.031 | 1.015~1.047 | <0.01 |
| UA(mmol/L) | 0.003 | 0.001 | 16.272 | 1.003 | 1.002~1.005 | <0.01 |
| ALB(g/L) | -0.048 | 0.026 | 3.345 | 0.953 | 0.906~1.003 | 0.067 |
| DD(μg/L) | 0 | 0 | 4.541 | 1.000 | 1.000~1.000 | 0.033 |
| 24 h尿蛋白定量(g/24 h) | 0.246 | 0.077 | 10.221 | 1.279 | 1.100~1.488 | 0.001 |
| PCT(μg/L) | -0.079 | 0.114 | 0.483 | 0.924 | 0.740~1.154 | 0.487 |
| CD4绝对计数(cells/μl) | -0.002 | 0.001 | 4.534 | 0.998 | 0.996~1.000 | 0.033 |
| BNP(ng/L) | 0 | 0 | 3.301 | 1.000 | 1.000~1.001 | 0.069 |
| 叶酸( μg/L) | -0.012 | 0.032 | 0.132 | 0.988 | 0.929~1.052 | 0.716 |
| 维生素B12(ng/L) | 0 | 0 | 0.119 | 1.000 | 0.999~1.001 | 0.730 |
| 结合珠蛋白(g/L) | -0.190 | 0.182 | 1.087 | 0.827 | 0.579~1.182 | 0.297 |
| 铁蛋白(μg/L) | 0 | 0 | 0.158 | 1.000 | 0.999~1.001 | 0.691 |
| 转铁蛋白(g/L) | 0.192 | 0.427 | 0.203 | 1.212 | 0.525~2.797 | 0.653 |
| 可溶性转铁蛋白受体(mg/L) | 0.216 | 0.315 | 0.472 | 1.241 | 0.670~2.301 | 0.492 |
| BVAS | 0.029 | 0.025 | 1.267 | 1.029 | 0.979~1.082 | 0.260 |
| FFS | 0.285 | 0.157 | 3.306 | 1.33 | 0.978~1.810 | 0.069 |
| CCI | 0.320 | 0.104 | 9.393 | 1.377 | 1.122~1.689 | 0.002 |
表5 AAV患者肾脏预后影响因素的单因素COX回归模型分析
Tab.5 Univariate COX regression model analysis of the influencing factors for renal prognosis in AAV patients
| 项目 | 回归系数 | 标准误 | Wald χ2值 | 风险比 | 95% | |
|---|---|---|---|---|---|---|
| 年龄 | -0.008 | 0.011 | 0.553 | 0.992 | 0.970~1.014 | 0.457 |
| 初诊HGB(g/L) | -0.025 | 0.008 | 9.874 | 0.975 | 0.960~0.991 | 0.002 |
| CRP(mg/L) | -0.002 | 0.003 | 0.455 | 0.998 | 0.992~1.004 | 0.500 |
| ESR(mm/h) | 0.003 | 0.004 | 0.623 | 1.003 | 0.996~1.010 | 0.430 |
| SCr(μmol/L) | 0.001 | 0 | 12.405 | 1.001 | 1.001~1.002 | <0.01 |
| eGFR[ml/(min·1.73 m2)] | -0.031 | 0.009 | 11.497 | 0.97 | 0.952~0.987 | 0.001 |
| BUN(mmol/L) | 0.030 | 0.008 | 14.352 | 1.031 | 1.015~1.047 | <0.01 |
| UA(mmol/L) | 0.003 | 0.001 | 16.272 | 1.003 | 1.002~1.005 | <0.01 |
| ALB(g/L) | -0.048 | 0.026 | 3.345 | 0.953 | 0.906~1.003 | 0.067 |
| DD(μg/L) | 0 | 0 | 4.541 | 1.000 | 1.000~1.000 | 0.033 |
| 24 h尿蛋白定量(g/24 h) | 0.246 | 0.077 | 10.221 | 1.279 | 1.100~1.488 | 0.001 |
| PCT(μg/L) | -0.079 | 0.114 | 0.483 | 0.924 | 0.740~1.154 | 0.487 |
| CD4绝对计数(cells/μl) | -0.002 | 0.001 | 4.534 | 0.998 | 0.996~1.000 | 0.033 |
| BNP(ng/L) | 0 | 0 | 3.301 | 1.000 | 1.000~1.001 | 0.069 |
| 叶酸( μg/L) | -0.012 | 0.032 | 0.132 | 0.988 | 0.929~1.052 | 0.716 |
| 维生素B12(ng/L) | 0 | 0 | 0.119 | 1.000 | 0.999~1.001 | 0.730 |
| 结合珠蛋白(g/L) | -0.190 | 0.182 | 1.087 | 0.827 | 0.579~1.182 | 0.297 |
| 铁蛋白(μg/L) | 0 | 0 | 0.158 | 1.000 | 0.999~1.001 | 0.691 |
| 转铁蛋白(g/L) | 0.192 | 0.427 | 0.203 | 1.212 | 0.525~2.797 | 0.653 |
| 可溶性转铁蛋白受体(mg/L) | 0.216 | 0.315 | 0.472 | 1.241 | 0.670~2.301 | 0.492 |
| BVAS | 0.029 | 0.025 | 1.267 | 1.029 | 0.979~1.082 | 0.260 |
| FFS | 0.285 | 0.157 | 3.306 | 1.33 | 0.978~1.810 | 0.069 |
| CCI | 0.320 | 0.104 | 9.393 | 1.377 | 1.122~1.689 | 0.002 |
| 项目 | 回归系数 | 标准误 | Wald χ2值 | 风险比 | 95% | |
|---|---|---|---|---|---|---|
| 年龄 | -0.069 | 0.032 | 4.697 | 0.934 | 0.877~0.993 | 0.030 |
| 初诊HGB(g/L) | -0.046 | 0.028 | 2.781 | 0.955 | 0.905~1.008 | 0.095 |
| SCr(μmol/L) | 0.004 | 0.001 | 8.070 | 1.004 | 1.001~1.007 | 0.005 |
| eGFR[ml/(min·1.73 m2)] | 0.024 | 0.031 | 0.573 | 1.024 | 0.963~1.089 | 0.449 |
| DD(μg/L) | 0 | 0 | 2.090 | 1.000 | 0.999~1.000 | 0.148 |
| 24 h尿蛋白定量(g/24 h) | 0.412 | 0.181 | 5.169 | 1.510 | 1.059~2.154 | 0.023 |
| CD4绝对计数(cells/μl) | 0 | 0.001 | 0.026 | 1.000 | 0.998~1.002 | 0.871 |
| CCI | -0.027 | 0.264 | 0.011 | 0.973 | 0.580~1.633 | 0.917 |
表6 AAV患者肾脏预后影响因素的多因素COX回归模型分析
Tab.6 Multivariate COX regression model analysis of the influencing factors for renal prognosis in AAV patients
| 项目 | 回归系数 | 标准误 | Wald χ2值 | 风险比 | 95% | |
|---|---|---|---|---|---|---|
| 年龄 | -0.069 | 0.032 | 4.697 | 0.934 | 0.877~0.993 | 0.030 |
| 初诊HGB(g/L) | -0.046 | 0.028 | 2.781 | 0.955 | 0.905~1.008 | 0.095 |
| SCr(μmol/L) | 0.004 | 0.001 | 8.070 | 1.004 | 1.001~1.007 | 0.005 |
| eGFR[ml/(min·1.73 m2)] | 0.024 | 0.031 | 0.573 | 1.024 | 0.963~1.089 | 0.449 |
| DD(μg/L) | 0 | 0 | 2.090 | 1.000 | 0.999~1.000 | 0.148 |
| 24 h尿蛋白定量(g/24 h) | 0.412 | 0.181 | 5.169 | 1.510 | 1.059~2.154 | 0.023 |
| CD4绝对计数(cells/μl) | 0 | 0.001 | 0.026 | 1.000 | 0.998~1.002 | 0.871 |
| CCI | -0.027 | 0.264 | 0.011 | 0.973 | 0.580~1.633 | 0.917 |
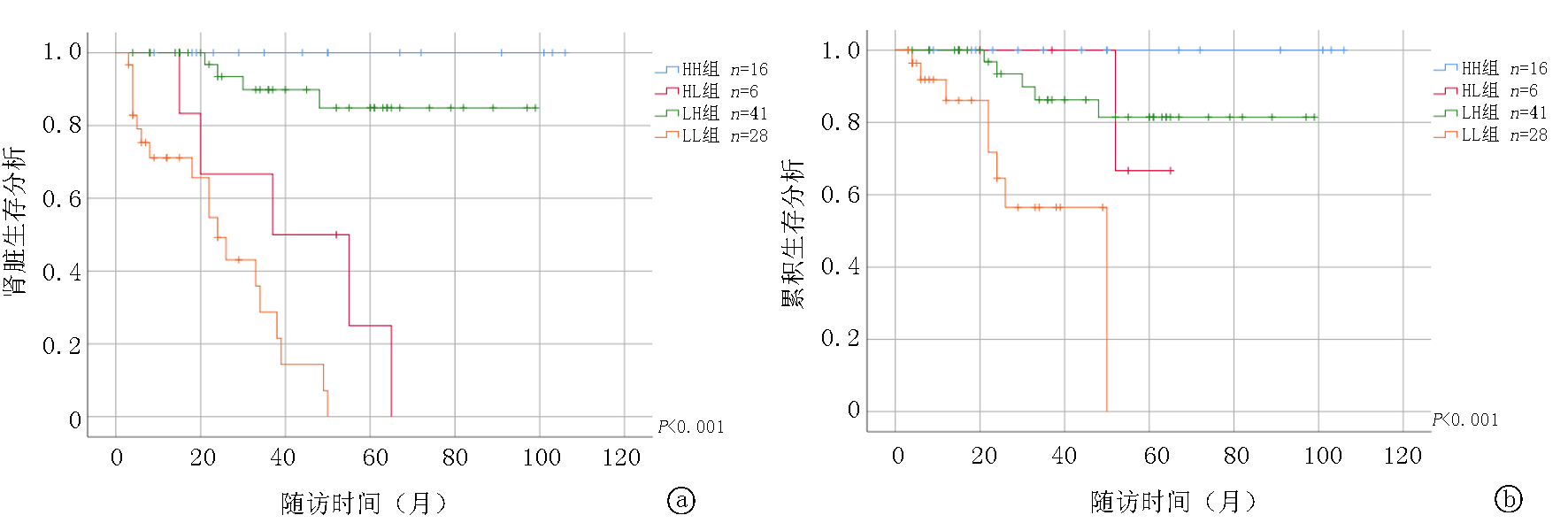
图5 依据HGB偏移分组的肾脏生存率和全因死亡率比较 a.根据初始及随访终点血红蛋白分组的肾脏生存率比较; b.根据初始及随访终点血红蛋白分组的全因死亡率比较
Fig.5 Comparison of renal survival rate and all-cause mortality based on HGB deviation grouping a.Comparison of renal survival rates based on HGB groups at the initial and follow-up endpoints;b.Comparison of all-cause mortality based on HGB groups at the initial and follow-up endpoints
| [1] | Wacka E, Nicikowski J, Jarmuzek P, et al. Anemia and its connections to inflammation in older adults: A review[J]. J Clin Med, 2024, 13(7):2049. doi: 10.3390/jcm13072049. |
| [2] |
Ciceri P, Cozzolino M. The emerging role of iron in heart failure and vascular calcification in CKD[J]. Clin Kidney J, 2021, 14(3): 739-745. doi: 10.1093/ckj/sfaa135.
pmid: 33777358 |
| [3] | 陈彤, 徐鹏程. 贫血在肾功能正常的抗中性粒细胞胞浆抗体相关血管炎中的意义[J]. 医学理论与实践, 2016, 29(18): 3169-3171. doi:10.19381/j.issn.1001-7585.2016.18.008. |
| [4] |
Chen T, Xu PC, Hu SY, et al. High serum hepcidin is associated with the occurrence of anemia in anti-myeloperoxidase antibody-associated vasculitis with normal kidney function: A cross-sectional study[J]. Rheumatol Int, 2019, 39(5): 851-857. doi: 10.1007/s00296-019-04292-x.
pmid: 30923957 |
| [5] | Kitani T, Kidokoro K, Nakata T, et al. Kidney vascular congestion exacerbates acute kidney injury in mice[J]. Kidney Int, 2022, 101(3): 551-562. doi: 10.1016/j.kint.2021.11.015. |
| [6] | Winterberg PD, Robertson JM, Kelleman MS, et al. T cells play a causal role in diastolic dysfunction during uremic cardiomyopathy[J]. J Am Soc Nephrol, 2019, 30(3): 407-420. doi: 10.1681/ASN.2017101138. |
| [7] | Lucientes-Continente L, Fernández-Juárez G, Márquez-Tirado B, et al. Complement alternative pathway determines disease susceptibility and severity in antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis[J]. Kidney Int, 2024, 105(1):177-188. doi:10.1016/j.kint.2023.10.013. |
| [8] |
Mollnes TE, Brekke OL, Fung M, et al. Essential role of the C5a receptor in E coli-induced oxidative burst and phagocytosis revealed by a novel lepirudin-based human whole blood model of inflammation[J]. Blood, 2002, 100(5): 1869-1877.
pmid: 12176911 |
| [9] |
Weiss G, Ganz T, Goodnough LT. Anemia of inflammation[J]. Blood, 2019, 133(1): 40-50. doi: 10.1182/blood-2018-06-856500.
pmid: 30401705 |
| [10] |
Wilson A, Yu HT, Goodnough LT, Nissenson AR. Prevalence and outcomes of anemia in rheumatoid arthritis: A systematic review of the literature[J]. Am J Med, 2004, 116 Suppl 7A: 50s-57 s. doi: 10.1016/j.amjmed.2003.12.012.
pmid: 15050886 |
| [11] |
Voulgarelis M, Kokori SI, Ioannidis JP, et al. Anaemia in systemic lupus erythematosus: Aetiological profile and the role of erythropoietin[J]. Ann Rheum Dis, 2000, 59(3): 217-222. doi: 10.1136/ard.59.3.217.
pmid: 10700431 |
| [12] | Nutritional anaemias. Report of a WHO scientific group[J]. World Health Organ Tech Rep Ser, 1968, 405: 5-37. |
| [13] | Camaschella C. Iron-deficiency anemia[J]. N Engl J Med, 2015, 372(19): 1832-1843. doi: 10.1056/NEJMra1401038. |
| [14] | 王一浩, 付蓉, 邵宗鸿. 炎症性贫血诊治新进展[J]. 中华医学杂志, 2021, 101(24): 1946-1948. doi: 10.3760/cma.j.cn112137-20201109-03039. |
| [15] | 孙雪峰. 《中国肾性贫血诊疗的临床实践指南》解读[J]. 中国实用内科杂志, 2021, 41(9):785-788. doi:10.19538/j.nk2021090107. |
| [16] |
Kutuby F, Wang S, Desai C, et al. Anemia of chronic kidney disease.[J]. Dis Mon, 2015, 61(10):421-424. doi:10.1016/j.disamonth.2015.08.002.
pmid: 26364946 |
| [17] | McCullough PA. Anemia of cardiorenal syndrome. Kidney Int Suppl (2011), 2021, 11(1):35-45. doi: 10.1016/j.kisu.2020.12.001. |
| [18] | 刘雪姣, 蔡建芳. 中国人群中的心肾贫血综合征研究[J]. 中国实用内科杂志, 2022, 42(2): 131-135. doi:10.19538/j.nk2022020109. |
| [19] | Fraenkel PG. Anemia of inflammation: A review[J]. Med Clin North Am, 2017, 101(2): 285-296. doi: 10.1016/j.mcna.2016.09.005. |
| [20] |
Mohamed AH, Ahmed AT, Al Abdulmonem W, et al. Interleukin-6 serves as a critical factor in various cancer progression and therapy[J]. Med Oncol, 2024, 41(7):182. doi: 10.1007/s12032-024-02422-5.
pmid: 38900329 |
| [21] |
Baier E, Kluge IA, Hakroush S, et al. Low hemoglobin levels are associated with Bowman's capsule rupture and peritubular capillaritis in ANCA-associated renal vasculitis: A link of vascular injury to anemia?[J]. J Nephrol, 2023, 36(8):2305-2316. doi: 10.1007/s40620-023-01748-z.
pmid: 37676636 |
| [22] | Kidney Disease: Improving Global Outcomes (KDIGO) ANCA Vasculitis Work Group. Corrigendum to “KDIGO 2024 clinical practice guideline for the management of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis.” kidney international, 2024, 105(3S):S71-S116[J]. Kidney Int, 2024, 106(1):160-163. doi: 10.1016/j.kint.2024.04.003. |
| [23] | Chalkia A, Jayne D. ANCA-associated vasculitis-treatment standard[J]. Nephrol Dial Transplant, 2024, 39(6):944-955. doi: 10.1093/ndt/gfad237. |
| [24] | Qi F, Hao J, Wei W. Impact of different ANCA serotypes on the long-term outcome of ANCA-associated vasculitis patients[J]. Ann Med, 2023, 55(2):12. doi: 10.1080/07853890.2023.2289614. |
| [25] | Liao QQ, Ren YF, Zhu KW, et al. Long-term prognostic factors in patients with antineutrophil cytoplasmic antibody-associated vasculitis: A 15-year multicenter retrospective study[J]. Front Immunol, 2022, 13:913667. DOI: 10.3389/fimmu.2022.913667. |
| [26] | Quartuccio L, Treppo E, Urso L, et al. Unmet needs in ANCA-associated vasculitis: Physicians' and patients' perspectives[J]. Front Immunol, 2023, 14:1112899. doi: 10.3389/fimmu.2023.1112899. |
| [27] |
Uzzo M, Maggiore U, Sala F, et al. Changing phenotypes and clinical outcomes over time in Microscopic Polyangiitis[J]. Kidney Int Rep, 2023, 8(10):2107-2116. doi: 10.1016/j.ekir.2023.07.008.
pmid: 37850011 |
| [28] | Wawrzycka-Adamczyk K, Korkosz M, Musiał J, et al. Relapse predictors in antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis[J]. Diagnostics, 2024, 14, (17):1849. doi: 10.3390/diagnostics14171849. |
| [29] | Sánchez Álamo B, Moi L, Bajema I, et al. Long-term outcomes and prognostic factors for survival of patients with ANCA-associated vasculitis[J]. Nephrol Dial Transplant, 2023, 38(7): 1655-1665. doi: 10.1093/ndt/gfac320. |
| [1] | 叶倩, 刘申香. H1抗组胺药与接受免疫检查点抑制剂治疗的肿瘤患者预后关系的meta分析[J]. 临床荟萃, 2025, 40(8): 684-688. |
| [2] | 庄蕙萃, 郭皓, 李贤, 崔东升. 血流感染合并脓毒症患者预后危险因素及其预测价值分析[J]. 临床荟萃, 2025, 40(8): 698-704. |
| [3] | 张宏涛, 钟美娇, 高敬洋, 李士杰, 于娜新, 范鑫, 陈立宁, 张扬, 王志奎, 边爱淑. HEP/SF比值对维持性腹膜透析患者贫血的评估价值[J]. 临床荟萃, 2025, 40(5): 434-438. |
| [4] | 赵雅静, 陶千山, 沈元元, 董毅. 地西他滨维持治疗对适合强化疗中低危急性髓细胞白血病患者生存的影响[J]. 临床荟萃, 2025, 40(5): 439-444. |
| [5] | 魏静, 崔清洋, 韩慧珍, 闫会丽, 刘庆生. 支气管肺发育不良合并肺动脉高压早产儿血清IL-33表达水平及其临床意义[J]. 临床荟萃, 2025, 40(5): 445-449. |
| [6] | 叶倩, 刘申香. D-二聚体与接受PD-1/PD-L1抑制剂治疗的晚期肿瘤患者长期预后的关系:一项Meta分析[J]. 临床荟萃, 2025, 40(2): 101-106. |
| [7] | 申帅洁, 陈荣梯, 朱嵩, 平芬. 乳酸脱氢酶在难治性肺炎支原体肺炎中的临床应用进展[J]. 临床荟萃, 2025, 40(2): 185-188. |
| [8] | 伍秋频, 严士为, 何筱胤, 李云, 陆丽菊, 吴怡. 儿童肝炎相关再生障碍性贫血2例及文献回顾[J]. 临床荟萃, 2024, 39(7): 640-643. |
| [9] | 庞樱容, 孙欣. sST2在心血管疾病中作用的研究进展[J]. 临床荟萃, 2024, 39(5): 460-465. |
| [10] | 王茜, 尹万红, 邹同娟, 铁馨, 朱俊臣, 陈侣林, 曾学英. 机械通气脓毒症患者肺部超声重力依赖失充气表型与不良预后的相关性[J]. 临床荟萃, 2024, 39(4): 314-319. |
| [11] | 宋梦姣, 王睿琪, 曹灿, 程光森, 刘羽, 李忠亮, 杨建豪. 血尿酸与首次急性缺血性脑卒中患者TOAST分型及预后的相关性[J]. 临床荟萃, 2024, 39(3): 216-221. |
| [12] | 赵金匣, 康慧慧, 张垚, 付生军, 孙鹏飞. 胃癌患者根治性切除术前血脂水平与预后的相关性[J]. 临床荟萃, 2024, 39(10): 889-895. |
| [13] | 赵旭辉, 黄小敏, 达德转, 许焱, 崔晓东, 李红玲. 基于生物信息学筛选影响胃癌患者预后的糖酵解相关基因[J]. 临床荟萃, 2024, 39(1): 20-29. |
| [14] | 刘丽丽, 袁宇婷, 赖耿良, 田川, 蓝翔, 叶中绿. 儿童急性淋巴细胞白血病第15天微小残留与预后的关系[J]. 临床荟萃, 2024, 39(1): 47-52. |
| [15] | 崔兰丹, 杨春燕. 脓毒症患者甲状腺激素的变化特点及研究进展[J]. 临床荟萃, 2024, 39(1): 70-74. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||